Ablative Therapy
(27) Irreversible Electroporation for Biliary Cystadenoma: A Case Report
Saturday, October 18, 2025
6:00 PM - 7:30 PM East Coast USA Time
Elizabeth Ruiz, BS – Research Associate, Miami Cancer Institute; Susan van der Lei, MD – Research Associate, Miami Cancer Institute; Govindarajan Narayanan, MD – Chief of Interventional Oncology, Miami Cancer Institute, Miami Cardiac and Vascular Institute
Purpose: This case study aims to demonstrate the safety, effectiveness, and technique of percutaneous irreversible electroporation (IRE) as a minimally invasive alternative in treating biliary cystadenoma (BCA), a rare benign liver lesion typically managed with surgical resection. IRE represents a non-thermal ablation modality that utilizes high-voltage, short electrical pulses to induce permanent nanopores in cell membranes, leading to apoptosis while preserving the extracellular matrix and critical surrounding anatomy.
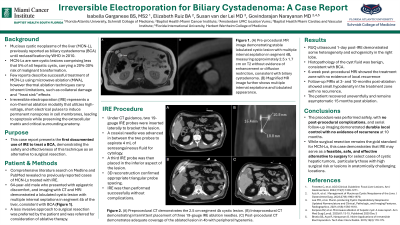
Material and Methods: 64-year-old male who presented with epigastric discomfort to outside facility underwent workup with MRI which revealed a 2.5 x 1.5 cm lobulated cystic lesion with multiple internal septations in segment 4B of the liver on T2, consistent with biliary cystadenoma. Patient preferred a less invasive approach to surgical excision and was referred for possible ablation. Plan for IRE was made. Under CT guidance, two 19-gauge IRE probes were inserted in parallel via a lateral approach to bracket the lesion. A coaxial needle was used to aspirate 4 mL of serosanguineous fluid for analysis. A third IRE probe was then placed in inferior aspect of the lesion. 3D reconstruction confirmed appropriate spacing of the 3 probes in a triangular configuration. IRE was performed successfully without complications.
Results: Post-procedure CT demonstrated adequate coverage of the ablated lesion in 4b with peripheral hyperemia. Histopathology of hepatic cyst fluid consistent with biliary cystadenoma. RUQ US 1-day post-IRE demonstrated no focal mass lesion or perihepatic fluid, some heterogeneity and echogenic foci in right lobe. 6-week follow-up MRI showed treatment zone with no evidence of liability. 10-month follow-up MRI showed small hypodensity in treatment zone with no evidence of local recurrence. Patient remains asymptomatic.
Conclusions: Biliary cystadenomas are rare cystic hepatic tumors typically treated with surgical resection to prevent malignant transformation. This case demonstrates that percutaneous IRE can be a safe and effective minimally invasive alternative, particularly in patients seeking nonsurgical options or when lesions are near bile ducts or vascular structures where thermal ablation poses higher risk. IRE preserves adjacent tissue integrity while achieving complete ablation, making it a promising approach in select cases. Further study is warranted to define long-term outcomes.
Material and Methods: 64-year-old male who presented with epigastric discomfort to outside facility underwent workup with MRI which revealed a 2.5 x 1.5 cm lobulated cystic lesion with multiple internal septations in segment 4B of the liver on T2, consistent with biliary cystadenoma. Patient preferred a less invasive approach to surgical excision and was referred for possible ablation. Plan for IRE was made. Under CT guidance, two 19-gauge IRE probes were inserted in parallel via a lateral approach to bracket the lesion. A coaxial needle was used to aspirate 4 mL of serosanguineous fluid for analysis. A third IRE probe was then placed in inferior aspect of the lesion. 3D reconstruction confirmed appropriate spacing of the 3 probes in a triangular configuration. IRE was performed successfully without complications.
Results: Post-procedure CT demonstrated adequate coverage of the ablated lesion in 4b with peripheral hyperemia. Histopathology of hepatic cyst fluid consistent with biliary cystadenoma. RUQ US 1-day post-IRE demonstrated no focal mass lesion or perihepatic fluid, some heterogeneity and echogenic foci in right lobe. 6-week follow-up MRI showed treatment zone with no evidence of liability. 10-month follow-up MRI showed small hypodensity in treatment zone with no evidence of local recurrence. Patient remains asymptomatic.
Conclusions: Biliary cystadenomas are rare cystic hepatic tumors typically treated with surgical resection to prevent malignant transformation. This case demonstrates that percutaneous IRE can be a safe and effective minimally invasive alternative, particularly in patients seeking nonsurgical options or when lesions are near bile ducts or vascular structures where thermal ablation poses higher risk. IRE preserves adjacent tissue integrity while achieving complete ablation, making it a promising approach in select cases. Further study is warranted to define long-term outcomes.
