Ablative Therapy
(81) Absorbable Gelatin Hydrodissection in Oncologic Thermal Ablations: Initial Outcomes
Sunday, October 19, 2025
9:32 AM - 9:42 AM East Coast USA Time
Eric Hoffer, MD – Section Chief, Interventional Radiology, Dartmouth-Hitchcock Medical Center
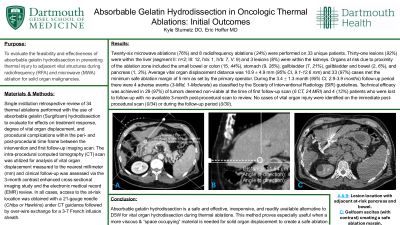
Purpose: To evaluate the feasibility and effectiveness of absorbable gelatin hydrodissection in preventing thermal injury to adjacent vital structures during radiofrequency (RFA) and microwave (MWA) ablation for solid organ malignancies.
Material and Methods: Single institution retrospective review of 34 thermal ablations performed with the use of absorbable gelatin (Surgifoam) hydrodissection to evaluate for effects on treatment response, degree of vital organ displacement, and procedural complications within the peri- and post-procedural time frame between the intervention and first follow-up imaging scan. The intra-procedural computed tomography (CT) scan was utilized for analysis of vital organ displacement measured to the nearest millimeter (mm) and clinical follow-up was assessed via the 3-month contrast enhanced cross-sectional imaging study and the electronic medical record (EMR) review. In all cases, access to the at-risk location was obtained with a 21-gauge needle (Chiba or Hawkins) under CT guidance followed by over-wire exchange for a 3-7 French infusion sheath.
Results: Twenty-six microwave ablations (76%) and 8 radiofrequency ablations (24%) were performed on 33 unique patients. Thirty-one lesions (92%) were within the liver (segment II: n=2; III: 12, IVa: 1, IVb: 7, V: 9) and 3 lesions (8%) were within the kidneys. Organs at risk due to proximity of the ablation zone included the small bowel or colon (15, 44%), stomach (9, 26%), gallbladder (7, 21%), gallbladder and bowel (2, 6%), and pancreas (1, 3%). Average vital organ displacement distance was 10.9 +/- 4.9 mm (95% CI, 9.1-12.6 mm) and 33 (97%) cases met the minimum safe ablation margin of 5 mm as set by the primary operator. During the 3.4 +/- 1.3 month (95% CI, 2.9-3.9 months) follow-up period there were 4 adverse events (3-Mild, 1-Moderate) as classified by the Society of Interventional Radiology (SIR) guidelines. Technical efficacy was achieved in 29 (97%) of tumors deemed non-viable at the time of first follow-up scan (6 CT, 24 MRI) and 4 (12%) patients who were lost to follow-up with no available 3-month post-procedural scan to review. No cases of vital organ injury were identified on the immediate post-procedural scan (0/34) or during the follow-up period (0/30).
Conclusions: Absorbable gelatin hydrodissection is a safe, effective, inexpensive, and readily available alternative to D5W for vital organ hydrodissection during thermal ablations.
Material and Methods: Single institution retrospective review of 34 thermal ablations performed with the use of absorbable gelatin (Surgifoam) hydrodissection to evaluate for effects on treatment response, degree of vital organ displacement, and procedural complications within the peri- and post-procedural time frame between the intervention and first follow-up imaging scan. The intra-procedural computed tomography (CT) scan was utilized for analysis of vital organ displacement measured to the nearest millimeter (mm) and clinical follow-up was assessed via the 3-month contrast enhanced cross-sectional imaging study and the electronic medical record (EMR) review. In all cases, access to the at-risk location was obtained with a 21-gauge needle (Chiba or Hawkins) under CT guidance followed by over-wire exchange for a 3-7 French infusion sheath.
Results: Twenty-six microwave ablations (76%) and 8 radiofrequency ablations (24%) were performed on 33 unique patients. Thirty-one lesions (92%) were within the liver (segment II: n=2; III: 12, IVa: 1, IVb: 7, V: 9) and 3 lesions (8%) were within the kidneys. Organs at risk due to proximity of the ablation zone included the small bowel or colon (15, 44%), stomach (9, 26%), gallbladder (7, 21%), gallbladder and bowel (2, 6%), and pancreas (1, 3%). Average vital organ displacement distance was 10.9 +/- 4.9 mm (95% CI, 9.1-12.6 mm) and 33 (97%) cases met the minimum safe ablation margin of 5 mm as set by the primary operator. During the 3.4 +/- 1.3 month (95% CI, 2.9-3.9 months) follow-up period there were 4 adverse events (3-Mild, 1-Moderate) as classified by the Society of Interventional Radiology (SIR) guidelines. Technical efficacy was achieved in 29 (97%) of tumors deemed non-viable at the time of first follow-up scan (6 CT, 24 MRI) and 4 (12%) patients who were lost to follow-up with no available 3-month post-procedural scan to review. No cases of vital organ injury were identified on the immediate post-procedural scan (0/34) or during the follow-up period (0/30).
Conclusions: Absorbable gelatin hydrodissection is a safe, effective, inexpensive, and readily available alternative to D5W for vital organ hydrodissection during thermal ablations.
