Molecular Targeted Therapy
(32) Refining Chemotherapy Decisions in Fertility-Preserving, Low-Risk ER+/HER2− Breast Cancer via ML Genomic Subgrouping
Saturday, October 18, 2025
6:00 PM - 7:30 PM East Coast USA Time
Curtis Tatsuoka, PhD – Assistant Professor, University of Maryland Greenebaum Comprehensive Cancer Center
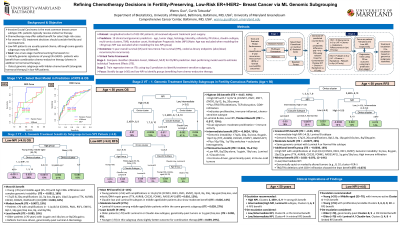
Purpose: Invasive ductal carcinoma (IDC) is the most common breast cancer subtype. While hormonal therapy is standard for ER+ disease, certain clinical and genomic features may favor adding chemotherapy. Using a machine learning framework, we aimed to (1) identify ER+/HER2− patients under 50 who benefit from combination therapy despite fertility preservation concerns, and (2) uncover genomic and immune signatures linked to benefit in low-NPI patients typically spared chemotherapy.
Material and Methods: We analyzed a longitudinal cohort of 423 IDC patients who received adjuvant treatment post-surgery, with 5-year overall survival (OS) as the outcome. A two-stage Virtual Twins machine learning framework was applied to identify subgroups benefiting from combination therapy (hormonal therapy + chemotherapy ± radiation) versus hormonal therapy alone, focusing on patients < 50 years and those with low NPI. In Stage 1, multiple classifiers (random forest, MLP, XGBoost) were compared for OS prediction; the best-performing model was used to estimate individual treatment effects (ITE) via counterfactuals. In Stage 2, a regression tree was trained on ITE using the top 10 predictive features to identify treatment-sensitive subgroups.
Results: OS was modeled using 19 clinical and multi-omics features (transcriptomics, CNV, mutations, methylation). In ER+/HER2− patients under age 50, those with the greatest overall survival benefit from combination therapy had high NPI (>5.0) and harbored amplifications at 11q13/14 (CCND1, PAK1, RSF1, EMSY), 8p12, 8q, and 20q—indicative of proliferative and endocrine-resistant biology. These tumors also exhibited TRG/TRA deletions and high CD8+ infiltration. Among low NPI ( < 4.0) patients, the most responsive subgroup showed 17q23 and 20q amplifications, high CD8+ infiltration, and complex genomic instability, including 5q loss, 8q gain, and 10p/12p gains involving mitotic regulators (TTK, AURKB, FOXM1, RAD51AP1), revealing hidden aggressiveness not captured by clinical risk alone. Conversely, patients with genomically quiet tumors—defined by isolated 8p12 amplification, 1q gain, 16q loss, 8q/20q gains—and Luminal A or Claudin-low subtypes exhibited minimal benefit, supporting de-escalation of therapy in this group.
Conclusions: Virtual twin modeling revealed that select ER+/HER2− IDC patients—despite low-risk or fertility-preserving profiles—derive benefit from adjuvant combination therapy when high-risk genomic features are present, supporting genomics-guided treatment escalation.
Material and Methods: We analyzed a longitudinal cohort of 423 IDC patients who received adjuvant treatment post-surgery, with 5-year overall survival (OS) as the outcome. A two-stage Virtual Twins machine learning framework was applied to identify subgroups benefiting from combination therapy (hormonal therapy + chemotherapy ± radiation) versus hormonal therapy alone, focusing on patients < 50 years and those with low NPI. In Stage 1, multiple classifiers (random forest, MLP, XGBoost) were compared for OS prediction; the best-performing model was used to estimate individual treatment effects (ITE) via counterfactuals. In Stage 2, a regression tree was trained on ITE using the top 10 predictive features to identify treatment-sensitive subgroups.
Results: OS was modeled using 19 clinical and multi-omics features (transcriptomics, CNV, mutations, methylation). In ER+/HER2− patients under age 50, those with the greatest overall survival benefit from combination therapy had high NPI (>5.0) and harbored amplifications at 11q13/14 (CCND1, PAK1, RSF1, EMSY), 8p12, 8q, and 20q—indicative of proliferative and endocrine-resistant biology. These tumors also exhibited TRG/TRA deletions and high CD8+ infiltration. Among low NPI ( < 4.0) patients, the most responsive subgroup showed 17q23 and 20q amplifications, high CD8+ infiltration, and complex genomic instability, including 5q loss, 8q gain, and 10p/12p gains involving mitotic regulators (TTK, AURKB, FOXM1, RAD51AP1), revealing hidden aggressiveness not captured by clinical risk alone. Conversely, patients with genomically quiet tumors—defined by isolated 8p12 amplification, 1q gain, 16q loss, 8q/20q gains—and Luminal A or Claudin-low subtypes exhibited minimal benefit, supporting de-escalation of therapy in this group.
Conclusions: Virtual twin modeling revealed that select ER+/HER2− IDC patients—despite low-risk or fertility-preserving profiles—derive benefit from adjuvant combination therapy when high-risk genomic features are present, supporting genomics-guided treatment escalation.
