Ablative Therapy
(66) Real-Time Monitoring of Ablation Zone Adequacy Using Intraprocedural CT in Thermal Ablation
Saturday, October 18, 2025
6:00 PM - 7:30 PM East Coast USA Time
Daniel Crawford, MD – Interventional Radiologist, Division of Vascular and Interventional Radiology, Mayo Clinic; Sadeer Alzubaidi, MD – Interventional Radiologist, Division of Vascular and Interventional Radiology, Mayo Clinic; Alex Wallace, MD – Interventional Radiologist, Division of Vascular and Interventional Radiology, Mayo Clinic; Merve Ozen, MD – Interventional Radiologist, Division of Vascular and Interventional Radiology, Mayo Clinic; Indravadan Patel, MD – Interventional Radiologist, Division of Vascular and Interventional Radiology, Mayo Clinic
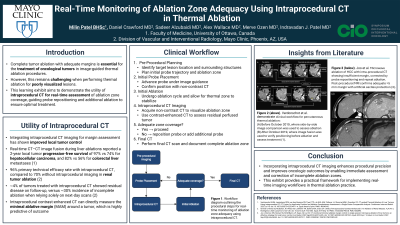
Purpose: Complete tumor ablation with adequate margins is essential for the treatment of oncological tumors in image-guided thermal ablation procedures. However, this remains challenging when performing thermal ablation in poorly visualized lesions. This learning exhibit aims to demonstrate the utility of intraprocedural CT for real-time assessment of ablation zone coverage, guiding probe repositioning and additional ablation to ensure optimal treatment.
Material and Methods: This exhibit highlights leveraging intraprocedural CT during microwave and radiofrequency ablation procedures. Using published literature along with institutional case experiences, key areas include:
1. Integration of non-contrast and contrast-enhanced CT to assess ablation margins
2. Techniques for real-time probe repositioning based on intraprocedural findings
3. Limitations of CT thermal zone assessment and future implications
4. Illustrative images and cases from insights from institutional experience
Results: Intraprocedural CT imaging enables real-time evaluation of ablation coverage, reducing the risk of residual tumor and repeat procedures. This modality allows for the visualization of the ablation zone to assess coverage, adapt probe placement or perform additional ablations to address uncovered zones and ultimately, improve treatment confidence and reduce local recurrence rates.
Conclusions: Incorporating intraprocedural CT imaging enhances procedural precision and improves oncologic outcomes by enabling immediate assessment and correction of incomplete ablation zones. This exhibit provides a practical framework for implementing real-time imaging workflows in thermal ablation practice.
Material and Methods: This exhibit highlights leveraging intraprocedural CT during microwave and radiofrequency ablation procedures. Using published literature along with institutional case experiences, key areas include:
1. Integration of non-contrast and contrast-enhanced CT to assess ablation margins
2. Techniques for real-time probe repositioning based on intraprocedural findings
3. Limitations of CT thermal zone assessment and future implications
4. Illustrative images and cases from insights from institutional experience
Results: Intraprocedural CT imaging enables real-time evaluation of ablation coverage, reducing the risk of residual tumor and repeat procedures. This modality allows for the visualization of the ablation zone to assess coverage, adapt probe placement or perform additional ablations to address uncovered zones and ultimately, improve treatment confidence and reduce local recurrence rates.
Conclusions: Incorporating intraprocedural CT imaging enhances procedural precision and improves oncologic outcomes by enabling immediate assessment and correction of incomplete ablation zones. This exhibit provides a practical framework for implementing real-time imaging workflows in thermal ablation practice.
