Ablative Therapy
(64) Managing Nerve Injury Risk During Cryoablation Procedures
Saturday, October 18, 2025
6:00 PM - 7:30 PM East Coast USA Time
Daniel Crawford, MD – Interventional Radiologist, Division of Vascular and Interventional Radiology, Mayo Clinic; Sadeer Alzubaidi, MD – Interventional Radiologist, Division of Vascular and Interventional Radiology, Mayo Clinic; Alex Wallace, MD – Interventional Radiologist, Division of Vascular and Interventional Radiology, Mayo Clinic; Merve Ozen, MD – Interventional Radiologist, Division of Vascular and Interventional Radiology, Mayo Clinic; Indravadan Patel, MD – Interventional Radiologist, Division of Vascular and Interventional Radiology, Mayo Clinic
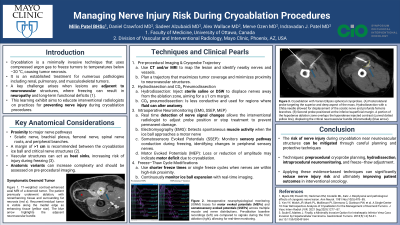
Purpose: Cryoablation is a minimally invasive technique that uses cryoprobes to deliver compressed gas (argon) to cool tumor tissue for purposes of necrosis to less than -20 °C. Cryoablation is a diverse treatment modality for tumors, including those found in the kidney, lung, and musculoskeletal system. However, when lesions are adjacent to neurovascular structures, the risk of cryo-induced neuropathy becomes a significant procedural challenge. This learning exhibit aims to educate interventional radiologists on practices for preventing nerve injury during cryoablation procedures.
Material and Methods: This exhibit reviews techniques and strategies, drawing from the current literature to reduce nerve injury during cryoablation. Techniques include:
1. Pre-procedural imaging and cryoprobe planning
2. Hydrodissection and CO₂ pneumodissection
3. Intraoperative neuromonitoring (IOM) using electromyogram (EMG), Somatosensory Evoked Potential (SSEP), and Motor evoked potential (MEP)
4. Freeze-thaw cycle modifications
Results: This exhibit will:
1. Identify anatomical locations and clinical scenarios where cryoablation poses a risk of nerve injury.
2. Describe procedural techniques such as preprocedural cryoprobe planning, intraprocedural monitoring, and hydrodissection that reduce the risk of cryo-induced damage.
3. Apply evidence-based strategies to modify freeze-thaw cycles and reduce long term complications.
Conclusions: Cryoablation offers a potential minimally invasive intervention for adequate localization of the tumor while preserving adjacent critical anatomical structures. Cryoablation near neurovascular structures requires planning and the application of protective techniques to avoid complications. This learning exhibit provides a comprehensive overview of approaches to mitigate nerve injury risk, ultimately improving patient outcomes in interventional oncology.
Material and Methods: This exhibit reviews techniques and strategies, drawing from the current literature to reduce nerve injury during cryoablation. Techniques include:
1. Pre-procedural imaging and cryoprobe planning
2. Hydrodissection and CO₂ pneumodissection
3. Intraoperative neuromonitoring (IOM) using electromyogram (EMG), Somatosensory Evoked Potential (SSEP), and Motor evoked potential (MEP)
4. Freeze-thaw cycle modifications
Results: This exhibit will:
1. Identify anatomical locations and clinical scenarios where cryoablation poses a risk of nerve injury.
2. Describe procedural techniques such as preprocedural cryoprobe planning, intraprocedural monitoring, and hydrodissection that reduce the risk of cryo-induced damage.
3. Apply evidence-based strategies to modify freeze-thaw cycles and reduce long term complications.
Conclusions: Cryoablation offers a potential minimally invasive intervention for adequate localization of the tumor while preserving adjacent critical anatomical structures. Cryoablation near neurovascular structures requires planning and the application of protective techniques to avoid complications. This learning exhibit provides a comprehensive overview of approaches to mitigate nerve injury risk, ultimately improving patient outcomes in interventional oncology.
