Other Organ Systems
(11) Direct Percutaneous N-Butyl Cyanoacrylate (nBCA) Glue Embolization for Abdominal Lymphatic Leakage and Chylous Ascites
Saturday, October 18, 2025
6:00 PM - 7:30 PM East Coast USA Time
Stephen Andrews, BS – Medical Student, Ohio State College of Medicine; Mina Makary, MD – Associate Professor, Ohio State University Department of Radiology
Purpose: 1) Gain insight into the anatomy and physiology of the thoracoabdominal lymphatic systems. 2) Explore causes of thoracoabdominal lymphatic leaks. 3) Review a treatment algorithm for managing lymphatic leaks, including medical, interventional, and surgical approaches. 4) Present a case highlighting the procedural aspects of intranodal lymphangiography and direct percutaneous glue embolization for a post-surgical abdominal lymphatic leakage.
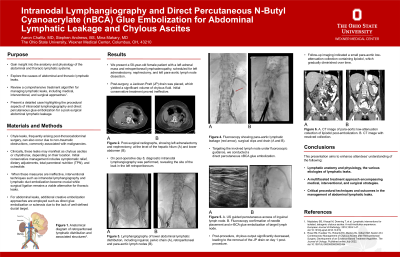
Material and Methods: Chyle leaks, frequently arising post-thoracoabdominal surgery, can also occur due to non-traumatic obstructions, commonly associated with malignancies. Clinically, leaks may manifest as chylous ascites or chylothorax, depending on their location. Initial conservative management includes symptomatic relief, dietary adjustments, total parenteral nutrition (TPN), and octreotide. When these measures are ineffective, interventional techniques such as intranodal lymphangiography and lymphatic duct embolization become crucial while surgical ligation remains a viable alternative for thoracic leaks. For abdominal leaks, additional embolization approaches are employed such as direct glue embolization or sclerosis due to the lack of well-defined ductal target.
Results: We present a 58-year-old female patient with metastatic left adrenal cancer of unknown primary with a left adrenal mass and retroperitoneal lymphadenopathy, who underwent adrenalectomy, nephrectomy, and left para-aortic lymph node dissection. Post-surgery, a Jackson Pratt (JP) drain was placed, which yielded a significant volume of chylous fluid. Initial conservative treatment proved ineffective. On post-operative day 8, intranodal lymphangiography was performed, revealing the site of the leak in the left retroperitoneum. Targeting the involved lymph node under fluoroscopic guidance, we conducted a direct percutaneous nBCA glue embolization. Post-procedure, chylous output significantly decreased, leading to the removal of the JP drain on day 1 post-procedure. Follow-up imaging indicated a small para-aortic low-attenuation collection containing lipiodol, which diminished over time.
Conclusions: This presentation will enhance attendees’ understanding of lymphatic anatomy and physiology, the various etiologies of lymphatic leaks, and a multifaceted treatment approach encompassing medical, interventional, and surgical strategies. Attendees will benefit from a case-rich discussion, illustrating critical procedural techniques and outcomes in the management of abdominal lymphatic leaks.
Material and Methods: Chyle leaks, frequently arising post-thoracoabdominal surgery, can also occur due to non-traumatic obstructions, commonly associated with malignancies. Clinically, leaks may manifest as chylous ascites or chylothorax, depending on their location. Initial conservative management includes symptomatic relief, dietary adjustments, total parenteral nutrition (TPN), and octreotide. When these measures are ineffective, interventional techniques such as intranodal lymphangiography and lymphatic duct embolization become crucial while surgical ligation remains a viable alternative for thoracic leaks. For abdominal leaks, additional embolization approaches are employed such as direct glue embolization or sclerosis due to the lack of well-defined ductal target.
Results: We present a 58-year-old female patient with metastatic left adrenal cancer of unknown primary with a left adrenal mass and retroperitoneal lymphadenopathy, who underwent adrenalectomy, nephrectomy, and left para-aortic lymph node dissection. Post-surgery, a Jackson Pratt (JP) drain was placed, which yielded a significant volume of chylous fluid. Initial conservative treatment proved ineffective. On post-operative day 8, intranodal lymphangiography was performed, revealing the site of the leak in the left retroperitoneum. Targeting the involved lymph node under fluoroscopic guidance, we conducted a direct percutaneous nBCA glue embolization. Post-procedure, chylous output significantly decreased, leading to the removal of the JP drain on day 1 post-procedure. Follow-up imaging indicated a small para-aortic low-attenuation collection containing lipiodol, which diminished over time.
Conclusions: This presentation will enhance attendees’ understanding of lymphatic anatomy and physiology, the various etiologies of lymphatic leaks, and a multifaceted treatment approach encompassing medical, interventional, and surgical strategies. Attendees will benefit from a case-rich discussion, illustrating critical procedural techniques and outcomes in the management of abdominal lymphatic leaks.
