Transcatheter Technologies
(10) Feasibility of the Protrieve Sheath for Embolic Protection During Venous Thrombectomy in Twenty-two Patients
Saturday, October 18, 2025
6:00 PM - 7:30 PM East Coast USA Time
Floyd Summers, BS – Medical Student, School of Medicine, University of Washington; Colvin Greenberg, MD – Resident, Radiology, University of Washington; Eric Monroe, MD – Associate Professor, Radiology, University of Wisconsin; Matthew Abad-Santos, MD – Assistant Professor, Radiology, University of Washington; David Shin, MD – Associate Professor, Radiology, University of Southern California; Jeffrey Chick, MD – Associate Professor, Radiology, University of Southern California; Mina Makary, MD – Associate Professor, Radiology, Ohio State University
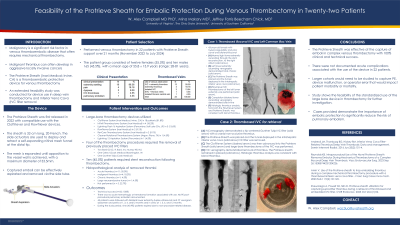
Purpose: Malignancy is a significant risk factor in the development of venous thromboembolic disease that often requires mechanical thrombectomy. The Protrieve Sheath (Inari Medical; Irvine, CA) is a thromboembolic protection device for venous thrombectomy. An extended feasibility study was conducted for device use in deep vein thrombectomy and IVC filter removal.
Material and Methods: Twenty-two patients, including twelve (55.5%) females and ten (45.5%) males (mean age 55.8 ± 13.9 years, range 28-81 years), underwent deep venous thrombectomy using the Protrieve sheath for embolic protection between November 2022 and July 2024 (21 months). The following demographic information was recorded: presenting symptoms, procedural indications, obstructed venous segments, Protrieve Sheath access and deployment sites, thrombectomy devices utilized, need for stent reconstruction, technical success, clinical success, procedural complications related to device access and deployment, clinically significant embolic events, procedure-related injury or death, mortality, and removed thrombi histological analyses. Technical success was defined as funnel deployment proximal to the thrombectomy site. Clinical success was defined as symptom improvement without venous thromboembolism.
Results: The most common presenting symptom was extremity swelling (n=19; 86.4%). Nine (40.9%) patients had malignant, and thirteen (59.1%) had benign etiologies of venous obstruction. Obstructed venous segments included the inferior vena cava (IVC) and lower extremity (n=13; 59.1%), isolated lower extremity (n=4; 18.2%), isolated inferior vena cava (IVC) (n=3; 13.6%), thoracic central veins and superior vena cava (n=1; 4.5%), and isolated thoracic central vein (n=1; 4.5%). Ten (45.5%) patients required stent reconstruction following thrombectomy. Technical success was achieved in all patients. Clinical success was achieved in 21 (95.5%) patients. No immediate device related adverse events including mesh maldeployment of the Protrieve Sheath or clinically significant embolic events, occurred. There were no significant bleeding events associated with use of the Protrieve sheath.
Conclusions: Use of the Protrieve Sheath during large-bore venous mechanical thrombectomy resulted in favorable technical and clinical outcomes without device-related adverse events or clinically significant thromboembolic events.
Material and Methods: Twenty-two patients, including twelve (55.5%) females and ten (45.5%) males (mean age 55.8 ± 13.9 years, range 28-81 years), underwent deep venous thrombectomy using the Protrieve sheath for embolic protection between November 2022 and July 2024 (21 months). The following demographic information was recorded: presenting symptoms, procedural indications, obstructed venous segments, Protrieve Sheath access and deployment sites, thrombectomy devices utilized, need for stent reconstruction, technical success, clinical success, procedural complications related to device access and deployment, clinically significant embolic events, procedure-related injury or death, mortality, and removed thrombi histological analyses. Technical success was defined as funnel deployment proximal to the thrombectomy site. Clinical success was defined as symptom improvement without venous thromboembolism.
Results: The most common presenting symptom was extremity swelling (n=19; 86.4%). Nine (40.9%) patients had malignant, and thirteen (59.1%) had benign etiologies of venous obstruction. Obstructed venous segments included the inferior vena cava (IVC) and lower extremity (n=13; 59.1%), isolated lower extremity (n=4; 18.2%), isolated inferior vena cava (IVC) (n=3; 13.6%), thoracic central veins and superior vena cava (n=1; 4.5%), and isolated thoracic central vein (n=1; 4.5%). Ten (45.5%) patients required stent reconstruction following thrombectomy. Technical success was achieved in all patients. Clinical success was achieved in 21 (95.5%) patients. No immediate device related adverse events including mesh maldeployment of the Protrieve Sheath or clinically significant embolic events, occurred. There were no significant bleeding events associated with use of the Protrieve sheath.
Conclusions: Use of the Protrieve Sheath during large-bore venous mechanical thrombectomy resulted in favorable technical and clinical outcomes without device-related adverse events or clinically significant thromboembolic events.
