Hepatocellular Carcinoma
(6) Enhancing Hepatocellular Carcinoma Outcomes: Integrating Immune Checkpoint Inhibitors with Interventional Oncology
Saturday, October 18, 2025
6:00 PM - 7:30 PM East Coast USA Time
Emily Pfahl, BS – Medical Student, The Ohio State University College of Medicine; Dannah Javens, BS – Medical Student, The Ohio State University College of Medicine; John Heyniger, BS – Medical Student, The Ohio State University College of Medicine; Mina Makary, MD – Division of Vascular & Interventional Radiology, Radiology, The Ohio State University Wexner Medical Center
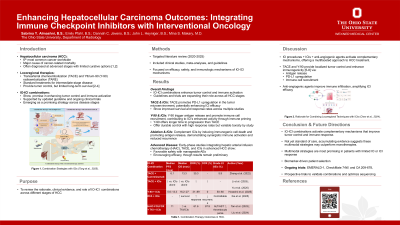
Purpose: Interventional oncology (IO) modalities such as transarterial chemoembolization (TACE), radioembolization (TARE), and ablation techniques are well-established in hepatocellular carcinoma (HCC) management. Combining IO with immune checkpoint inhibitors (ICIs) may potentiate local and systemic antitumor responses. This review assesses the rationale, clinical evidence, and evolving role of IO-ICI combinations across HCC stages.
Material and Methods: A targeted literature review of clinical studies, meta-analyses, and guidelines published from 2020 to 2025 was performed. Studies were selected for relevance to IO-ICI combinations in HCC, with emphasis on methodological quality, efficacy, safety, and proposed immunologic mechanisms.
Results: IO-ICI combinations show promise in enhancing tumor control and immune activation. Guidelines reflect their expanding role, with ICIs increasingly used across all HCC stages and lines of therapy. TARE, used in intermediate and select advanced-stage disease, demonstrates immunogenic potential and is thought to sensitize tumors to ICIs. Some studies suggest TARE may be more immunogenic than TACE, with improved disease control. TACE remains central in intermediate-stage HCC and is increasingly paired with ICIs, particularly in patients with suboptimal response to monotherapy. Emerging evidence indicates that both TACE and ablation may synergize with ICIs through mechanisms such as immunogenic cell death and antigen release. In advanced HCC, novel strategies integrating hepatic arterial infusion chemotherapy (HAIC), TACE, and ICIs are under investigation, with early-phase studies reporting safety and preliminary efficacy. Despite heterogeneity in study design and patient selection, IO-ICI combinations consistently show potential in overcoming resistance to monotherapy.
Conclusions: IO-ICI combinations activate complementary mechanisms that improve tumor control and immune response. While not yet standard of care, accumulating evidence suggests these multimodal strategies may outperform monotherapies, particularly in patients with limited response to IO or ICI alone. Ongoing trials, including EMERALD-1, CheckMate 74W, and CA 209-678, will be essential to validate these findings and refine therapeutic algorithms.
Material and Methods: A targeted literature review of clinical studies, meta-analyses, and guidelines published from 2020 to 2025 was performed. Studies were selected for relevance to IO-ICI combinations in HCC, with emphasis on methodological quality, efficacy, safety, and proposed immunologic mechanisms.
Results: IO-ICI combinations show promise in enhancing tumor control and immune activation. Guidelines reflect their expanding role, with ICIs increasingly used across all HCC stages and lines of therapy. TARE, used in intermediate and select advanced-stage disease, demonstrates immunogenic potential and is thought to sensitize tumors to ICIs. Some studies suggest TARE may be more immunogenic than TACE, with improved disease control. TACE remains central in intermediate-stage HCC and is increasingly paired with ICIs, particularly in patients with suboptimal response to monotherapy. Emerging evidence indicates that both TACE and ablation may synergize with ICIs through mechanisms such as immunogenic cell death and antigen release. In advanced HCC, novel strategies integrating hepatic arterial infusion chemotherapy (HAIC), TACE, and ICIs are under investigation, with early-phase studies reporting safety and preliminary efficacy. Despite heterogeneity in study design and patient selection, IO-ICI combinations consistently show potential in overcoming resistance to monotherapy.
Conclusions: IO-ICI combinations activate complementary mechanisms that improve tumor control and immune response. While not yet standard of care, accumulating evidence suggests these multimodal strategies may outperform monotherapies, particularly in patients with limited response to IO or ICI alone. Ongoing trials, including EMERALD-1, CheckMate 74W, and CA 209-678, will be essential to validate these findings and refine therapeutic algorithms.
