Radiation Therapy Alone Versus Radiation Therapy Plus Radiofrequency Ablation/Vertebral Augmentation for Painful Spine Metastasis: A Phase 2 Randomized Controlled Trial
(49) Radiation Therapy Alone Versus Radiation Therapy Plus Radiofrequency Ablation/Vertebral Augmentation for Painful Spine Metastasis: A Phase 2 Randomized Controlled Trial
Sunday, October 19, 2025
9:24 AM - 9:32 AM East Coast USA Time
Omer Gal, MD; Haley Appel, BA; Maria Carolina Avendano, BS; Antoinette M Pimentel, BS; Amy K Starosciak, PhD; Muni Rubens, PhD; Mukesh Roy, Ph; Dilanis Perche, MD; Cristina I Pow-Sang, BS; Fabiana Milosevic; Ramon F Cruz, BSN; Alex Kudryashev, MS; Matthew D Hall, MD; Ana Botero, MD; Minesh P Mehta, MD; Justin M Sporrer, MD; Brian Schiro, MD
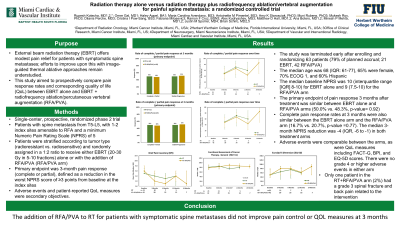
Purpose: Radiation therapy (RT) offers modest pain relief for patients with symptomatic spine metastases. This study aimed to compare pain response rates and corresponding quality of life (QOL) between standard of care RT alone or radiofrequency ablation/percutaneous vertebral augmentation (RFA/PVA) followed by RT.
Material and Methods: In this single-center, prospective, randomized phase 2 trial (NCT04375891) we enrolled patients with spine metastasis from T5-L5, with 1-2 index sites amenable to RFA and a minimum Numeric Pain Rating Scale (NPRS) of 5. Patients were stratified according to tumor type (radioresistant vs. radiosensitive) and randomly assigned in a 1:2 ratio to receive either RT alone, or RT with the addition of RFA/PVA. The primary endpoint was pain response at 3-months after treatment. Secondary endpoints included rapidity and duration of pain response, adverse events, and QOL measures.
Results: The study was terminated early after enrolling and randomizing 63 patients (79% of planned accrual; 21 RT alone, 42 RT+RFA/PVA). The median baseline NPRS was 10 (interquartile range [IQR] 8-10) for RT alone and 9 (7.5-10) for RT+RFA/PVA. The primary endpoint of pain control 3 months after treatment was similar between the RT alone and RT+RFA/PVA arms (50% vs. 48%, p-value= 0.92). Complete pain response rates at 3 months were also similar in the RT alone and RT+RFA/PVA arms (17% vs. 21%, p-value =0.77). The 3-month median NPRS reduction was -4 (IQR, -6 to -1) in both the RT alone and the RT+RFA/PVA arms. Secondary efficacy endpoints and toxicity rates were comparable between the groups. Overall QOL measures including FACT-G, BPI, and EQ-5D scores were also similar between the two treatment arms.
Conclusions: The addition of RFA/PVA to RT for patients with symptomatic spine metastases did not improve pain control or QOL measures at 3 months.
Material and Methods: In this single-center, prospective, randomized phase 2 trial (NCT04375891) we enrolled patients with spine metastasis from T5-L5, with 1-2 index sites amenable to RFA and a minimum Numeric Pain Rating Scale (NPRS) of 5. Patients were stratified according to tumor type (radioresistant vs. radiosensitive) and randomly assigned in a 1:2 ratio to receive either RT alone, or RT with the addition of RFA/PVA. The primary endpoint was pain response at 3-months after treatment. Secondary endpoints included rapidity and duration of pain response, adverse events, and QOL measures.
Results: The study was terminated early after enrolling and randomizing 63 patients (79% of planned accrual; 21 RT alone, 42 RT+RFA/PVA). The median baseline NPRS was 10 (interquartile range [IQR] 8-10) for RT alone and 9 (7.5-10) for RT+RFA/PVA. The primary endpoint of pain control 3 months after treatment was similar between the RT alone and RT+RFA/PVA arms (50% vs. 48%, p-value= 0.92). Complete pain response rates at 3 months were also similar in the RT alone and RT+RFA/PVA arms (17% vs. 21%, p-value =0.77). The 3-month median NPRS reduction was -4 (IQR, -6 to -1) in both the RT alone and the RT+RFA/PVA arms. Secondary efficacy endpoints and toxicity rates were comparable between the groups. Overall QOL measures including FACT-G, BPI, and EQ-5D scores were also similar between the two treatment arms.
Conclusions: The addition of RFA/PVA to RT for patients with symptomatic spine metastases did not improve pain control or QOL measures at 3 months.
