Radioembolization
(17) Radiation Segmentectomy vs Lobectomy Techniques: Precision Approaches in Y-90 Therapy of Hepatocellular Carcinoma
Saturday, October 18, 2025
6:00 PM - 7:30 PM East Coast USA Time
Israel Ailemen, BS – Medical Student, The Ohio State University College of Medicine; Elliott Fite, MS – Medical Student, The Ohio State University College of Medicine; Mina Makary, MD – Associate Clinical Professor of Radiology, Department of Radiology, The Ohio State University Medical Center
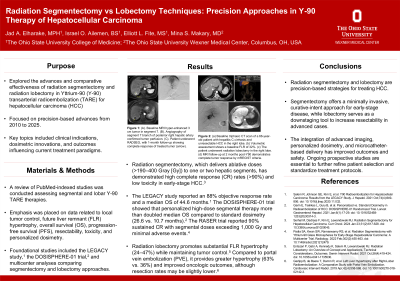
Purpose: The purpose of this exhibit was to explore the advances and effectiveness of radiation segmentectomy and radiation lobectomy in Yttrium-90 (Y-90) transarterial radioembolization (TARE) for hepatocellular carcinoma (HCC). Key topics included clinical indications, dosimetry, and current treatments.
Material and Methods: A review of PubMed-indexed studies was conducted, encompassing randomized trials, cohort studies, and large case series studies assessing segmental and lobar Y-90 TARE therapies. Emphasis was placed on data related to local tumor control, overall survival (OS), resectability, toxicity, and personalized dosimetry. Foundational studies included the LEGACY study, the DOSISPHERE-01 trial, and multicenter analyses comparing segmentectomy and lobectomy.
Results: Radiation segmentectomy demonstrated high complete response (CR) rates (>90%) and low toxicity in early-stage HCC. The LEGACY study reported an 88% objective response rate and a median OS of 44.6 months. The DOSISPHERE-01 trial showed that personalized high-dose segmental therapy more than doubled median OS compared to standard dosimetry (26.6 vs. 10.7 months). The RASER trial reported 90% sustained CR with segmental doses exceeding 1,000 Gy and minimal adverse events.
Radiation lobectomy promotes substantial FLR hypertrophy (24–47%) while maintaining tumor control [5]. Compared to portal vein embolization (PVE), it provides greater hypertrophy (63% vs. 36%) and improved oncologic outcomes. Systematic reviews and institutional studies support its use in downstaging and as a bridge to resection or transplantation.
Personalized dosimetry is central to both techniques. Advances in cone-beam computed tomography, single-photon emission computed tomography, and same-day mapping have improved lesion targeting. Techniques such as flow diversion and multicompartment modeling further enhance precision, as shown in recent interventional radiology trials.
Conclusions: Radiation segmentectomy and lobectomy are precision-based strategies for treating HCC. Segmentectomy offers a curative-intent approach for early-stage disease, while lobectomy serves as a downstaging tool to increase resectability in advanced cases. The integration of advanced imaging, personalized dosimetry, and microcatheter-based delivery has improved outcomes and safety. Ongoing studies are essential to further standardize treatment protocols.
Material and Methods: A review of PubMed-indexed studies was conducted, encompassing randomized trials, cohort studies, and large case series studies assessing segmental and lobar Y-90 TARE therapies. Emphasis was placed on data related to local tumor control, overall survival (OS), resectability, toxicity, and personalized dosimetry. Foundational studies included the LEGACY study, the DOSISPHERE-01 trial, and multicenter analyses comparing segmentectomy and lobectomy.
Results: Radiation segmentectomy demonstrated high complete response (CR) rates (>90%) and low toxicity in early-stage HCC. The LEGACY study reported an 88% objective response rate and a median OS of 44.6 months. The DOSISPHERE-01 trial showed that personalized high-dose segmental therapy more than doubled median OS compared to standard dosimetry (26.6 vs. 10.7 months). The RASER trial reported 90% sustained CR with segmental doses exceeding 1,000 Gy and minimal adverse events.
Radiation lobectomy promotes substantial FLR hypertrophy (24–47%) while maintaining tumor control [5]. Compared to portal vein embolization (PVE), it provides greater hypertrophy (63% vs. 36%) and improved oncologic outcomes. Systematic reviews and institutional studies support its use in downstaging and as a bridge to resection or transplantation.
Personalized dosimetry is central to both techniques. Advances in cone-beam computed tomography, single-photon emission computed tomography, and same-day mapping have improved lesion targeting. Techniques such as flow diversion and multicompartment modeling further enhance precision, as shown in recent interventional radiology trials.
Conclusions: Radiation segmentectomy and lobectomy are precision-based strategies for treating HCC. Segmentectomy offers a curative-intent approach for early-stage disease, while lobectomy serves as a downstaging tool to increase resectability in advanced cases. The integration of advanced imaging, personalized dosimetry, and microcatheter-based delivery has improved outcomes and safety. Ongoing studies are essential to further standardize treatment protocols.
