Chemoembolizaton/Drug-Eluting Embolics
(73) Transarterial Therapy in Non-Hepatocellular Carcinoma Liver Tumors: Expanding Indications and Evidence Base
Saturday, October 18, 2025
6:00 PM - 7:30 PM East Coast USA Time
Alex Rudich, BS – Medical Student, The Ohio State University College of Medicine; Jenish Venancius, MPH – Medical Student, The Ohio State University College of Medicine; Elliott Fite, MS – Medical Student, The Ohio State University College of Medicine; Mina Makary, MD – Associate Clinical Professor of Radiology, Department of Radiology, The Ohio State University Medical Center
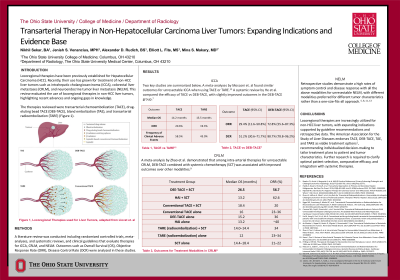
Purpose: Locoregional therapies including transarterial chemoembolization (TACE), drug-eluting bead TACE (DEB-TACE), bland embolization (TAE), and transarterial radioembolization (TARE) have been previously established for hepatocellular carcinoma (HCC). Recently, their use has grown for treatment of non-HCC liver tumors such as intrahepatic cholangiocarcinoma (iCCA), colorectal liver metastases (CRLM), and neuroendocrine tumor liver metastasis (NELM). This review evaluated the use of locoregional therapies in non-HCC liver tumors, highlighting recent advances and ongoing gaps in knowledge.
Material and Methods: A literature review was conducted using PubMed, Embase, Web of Science, and the Cochrane Library. The search included randomized controlled trials, meta-analyses, and systematic reviews, and clinical guidelines published up to June 2025 that evaluate therapies for iCCA, CRLM, and NELM.
Results: For unresectable iCCA, studies have not yet compared transarterial therapies to systemic ones. Meta-analyses have suggested that treatment with TACE has an Objective Response Rate (ORR) of 20.6% while treatment with TARE has one of 19.3%. Both modalities had a negligible survival difference of 14.2 months and 13.5 respectively (95% CI 11.4-16.1), with TACE having more clinical adverse effects (58.5% vs 43%). When comparing TACE to DEB-TACE, a systematic review found an ORR of 29.4% with TACE and 51.2% with DEB-TACE. A meta-analysis examining various treatment modalities on CRLM demonstrated an Overall Survival (OS) of 26.5 months for DEB-TACE combined with systemic chemotherapy, as opposed to 15.2 months with TACE, and 10.7 with TARE. Retrospective studies demonstrate a high rates of symptom control and disease response with all the above modalities for unresectable NELM, with different modalities preferred for different tumor characteristics.
Conclusions: Locoregional therapies are increasingly utilized for non-HCC liver tumors, with expanding indications supported by guideline recommendations and retrospective data. The American Association for the Study of Liver Diseases endorses TACE, DEB-TACE, TAE, and TARE as viable treatment options1, recommending individualized decision-making to tailor treatment plans to patient and tumor characteristics. Further research is required to clarify optimal patient selection, comparative efficacy, and integration with systemic therapies.
Material and Methods: A literature review was conducted using PubMed, Embase, Web of Science, and the Cochrane Library. The search included randomized controlled trials, meta-analyses, and systematic reviews, and clinical guidelines published up to June 2025 that evaluate therapies for iCCA, CRLM, and NELM.
Results: For unresectable iCCA, studies have not yet compared transarterial therapies to systemic ones. Meta-analyses have suggested that treatment with TACE has an Objective Response Rate (ORR) of 20.6% while treatment with TARE has one of 19.3%. Both modalities had a negligible survival difference of 14.2 months and 13.5 respectively (95% CI 11.4-16.1), with TACE having more clinical adverse effects (58.5% vs 43%). When comparing TACE to DEB-TACE, a systematic review found an ORR of 29.4% with TACE and 51.2% with DEB-TACE. A meta-analysis examining various treatment modalities on CRLM demonstrated an Overall Survival (OS) of 26.5 months for DEB-TACE combined with systemic chemotherapy, as opposed to 15.2 months with TACE, and 10.7 with TARE. Retrospective studies demonstrate a high rates of symptom control and disease response with all the above modalities for unresectable NELM, with different modalities preferred for different tumor characteristics.
Conclusions: Locoregional therapies are increasingly utilized for non-HCC liver tumors, with expanding indications supported by guideline recommendations and retrospective data. The American Association for the Study of Liver Diseases endorses TACE, DEB-TACE, TAE, and TARE as viable treatment options1, recommending individualized decision-making to tailor treatment plans to patient and tumor characteristics. Further research is required to clarify optimal patient selection, comparative efficacy, and integration with systemic therapies.
