Hepatocellular Carcinoma
(76) TACE with Locally Injected Immunotherapy for Hepatocellular Carcinoma: An Area of Untapped Potential
Saturday, October 18, 2025
6:00 PM - 7:30 PM East Coast USA Time
Jenish Venancius, MPH – Medical Student, The Ohio State University College of Medicine; Alex Rudich, BS – Medical Student, The Ohio State University College of Medicine; Elliott Fite, MS – Medical Student, The Ohio State University College of Medicine; Mina Makary, MD – Associate Clinical Professor of Radiology, Department of Radiology, The Ohio State University Medical Center
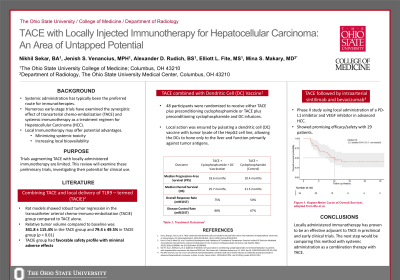
Purpose: Systemic administration has typically been the preferred route for immunotherapies, and numerous early-stage trials have examined the synergistic effect of transarterial chemo-embolization (TACE) and systemic immunotherapy as a treatment regimen for Hepatocellular Carcinoma (HCC). Thus far, trials augmenting TACE with locally administered immunotherapy are limited. This review will examine these preliminary trials, investigating their potential for clinical use.
Material and Methods: A systematic literature review was conducted evaluating clinical trials that examined a combined approach of local immunotherapy and TACE for HCC on PubMed, Embase, and Cochrane libraries. Systemic immunotherapies were excluded from search criteria.
Results: Three trials were found that met the search criteria. A preclinical trial examining in-vitro and in-vivo rat models augmented TACE with an adjuvant TLR-9 inhibitor (CpG oligodeoxynucleotide) in a therapy termed transcatheter arterial chemo‐immuno‐embolization (TACIE). In the rat models, TACIE both had a favorable side effect profile and caused HCC nodule regression. 17 ± 6 HCC nodules larger than 1 mm in diameter were found in the no‐treatment control group, 11 ± 3 in the TACE group, and 3 ± 2 in the TACIE group. Trials have translated this approach to the clinical world as well. A phase II trial administered intraarterial sintilimab and bevacizumab immediately after TACE in patients with advanced HCC. The study reported an objective response rate (ORR) of 70.6% with minimal adverse effects. Another such trial ensured local action by pulsating a dendritic cell (DC) vaccine with tumor lysate of the HepG2 cell line, allowing the DCs to hone only to the liver and function primarily against tumor antigens. When combined with TACE in patients with intermediate-stage HCC, progression-free survival in the treatment group was significantly improved: 18.6 vs 10.4 months (p = 0.02).
Conclusions: Locally administered immunotherapy has proven to be an effective adjuvant to TACE in preclinical and early clinical trials. This approach allows for increased immune response and an improved safety profile, supporting the rationale for further clinical development.
Material and Methods: A systematic literature review was conducted evaluating clinical trials that examined a combined approach of local immunotherapy and TACE for HCC on PubMed, Embase, and Cochrane libraries. Systemic immunotherapies were excluded from search criteria.
Results: Three trials were found that met the search criteria. A preclinical trial examining in-vitro and in-vivo rat models augmented TACE with an adjuvant TLR-9 inhibitor (CpG oligodeoxynucleotide) in a therapy termed transcatheter arterial chemo‐immuno‐embolization (TACIE). In the rat models, TACIE both had a favorable side effect profile and caused HCC nodule regression. 17 ± 6 HCC nodules larger than 1 mm in diameter were found in the no‐treatment control group, 11 ± 3 in the TACE group, and 3 ± 2 in the TACIE group. Trials have translated this approach to the clinical world as well. A phase II trial administered intraarterial sintilimab and bevacizumab immediately after TACE in patients with advanced HCC. The study reported an objective response rate (ORR) of 70.6% with minimal adverse effects. Another such trial ensured local action by pulsating a dendritic cell (DC) vaccine with tumor lysate of the HepG2 cell line, allowing the DCs to hone only to the liver and function primarily against tumor antigens. When combined with TACE in patients with intermediate-stage HCC, progression-free survival in the treatment group was significantly improved: 18.6 vs 10.4 months (p = 0.02).
Conclusions: Locally administered immunotherapy has proven to be an effective adjuvant to TACE in preclinical and early clinical trials. This approach allows for increased immune response and an improved safety profile, supporting the rationale for further clinical development.
