Chemoembolizaton/Drug-Eluting Embolics
(89) Transarterial Therapy in Bone Metastases: Evidence for Pain Palliation, Local Control, and Perioperative Outcomes
Saturday, October 18, 2025
6:00 PM - 7:30 PM East Coast USA Time
Alex Rudich, BS – Medical Student, The Ohio State University College of Medicine; Nikhil Sekar, BA – Medical Student, The Ohio State University College of Medicine; Elliott Fite, MS – Medical Student, The Ohio State University College of Medicine; Mina Makary, MD – Associate Clinical Professor of Radiology, Department of Radiology, The Ohio State University Medical Center
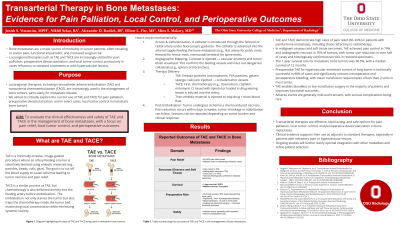
Purpose: Locoregional therapies, including transcatheter arterial embolization (TAE) and transarterial chemoembolization (TACE), are increasingly used in the management of bone tumors, particularly for metastatic disease. This abstract will explore the current use of TAE and TACE for pain palliation, preoperative devascularization, and in select cases, local tumor control in metastatic bone tumors.
Material and Methods: A literature review was conducted using PubMed, Scopus, Web of Science, Medline Plus, and the Cochrane Library, including systematic reviews, retrospective and prospective studies, and technical reports published through 2024. Key studies evaluated TAE and TACE for bone metastases including pain management, surgical blood loss reduction, and tumor response.
Results: TAE and TACE demonstrate high rates of pain relief (60–92%) in patients with painful bone metastases, including those refractory to radiotherapy. In malignant osseous and soft tissue sarcomas, TAE achieved pain control in 79% and radiographic necrosis in 76% of tumors, with tumor size reduction in over half of cases and histologically confirmed necrosis in resected specimens. The 1-year survival rate for metastatic bone tumors was 38.9%, with a median survival of 12 months. Preoperative TAE for hypervascular metastatic tumors of long bones is technically successful in 96% of cases and significantly reduces intraoperative and postoperative bleeding, with mean transfusion requirements of less than 2 units in most series. TAE enables bloodless or low-transfusion surgery in the majority of patients and improves functional outcomes. Adverse events are generally mild and transient, with serious complications being rare.
Conclusions: TAE or TACE are effective options for the management of bone tumors, particularly for pain palliation and preoperative devascularization. Clinical evidence supports its use as an adjunct to standard therapies, especially in patients with refractory pain or hypervascular lesions. Ongoing studies will further clarify the optimal integration of TAE and TACE with other modalities.
Material and Methods: A literature review was conducted using PubMed, Scopus, Web of Science, Medline Plus, and the Cochrane Library, including systematic reviews, retrospective and prospective studies, and technical reports published through 2024. Key studies evaluated TAE and TACE for bone metastases including pain management, surgical blood loss reduction, and tumor response.
Results: TAE and TACE demonstrate high rates of pain relief (60–92%) in patients with painful bone metastases, including those refractory to radiotherapy. In malignant osseous and soft tissue sarcomas, TAE achieved pain control in 79% and radiographic necrosis in 76% of tumors, with tumor size reduction in over half of cases and histologically confirmed necrosis in resected specimens. The 1-year survival rate for metastatic bone tumors was 38.9%, with a median survival of 12 months. Preoperative TAE for hypervascular metastatic tumors of long bones is technically successful in 96% of cases and significantly reduces intraoperative and postoperative bleeding, with mean transfusion requirements of less than 2 units in most series. TAE enables bloodless or low-transfusion surgery in the majority of patients and improves functional outcomes. Adverse events are generally mild and transient, with serious complications being rare.
Conclusions: TAE or TACE are effective options for the management of bone tumors, particularly for pain palliation and preoperative devascularization. Clinical evidence supports its use as an adjunct to standard therapies, especially in patients with refractory pain or hypervascular lesions. Ongoing studies will further clarify the optimal integration of TAE and TACE with other modalities.
