Chemoembolizaton/Drug-Eluting Embolics
(25) Optimizing Patient Selection for Locoregional Therapies in HCC: A Comparative Overview of TACE and TARE
Saturday, October 18, 2025
6:00 PM - 7:30 PM East Coast USA Time
Jad Elharake, MPH – Medical Student, The Ohio State University College of Medicine; Israel Ailemen, BS – Medical Student, The Ohio State University College of Medicine; Mina Makary, MD – Associate Clinical Professor of Radiology, Department of Radiology, The Ohio State University Medical Center
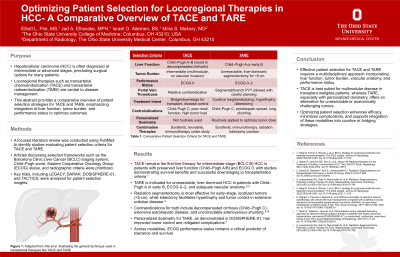
Purpose: Hepatocellular carcinoma (HCC) is often diagnosed at intermediate or advanced stages, precluding surgical options for many patients. Locoregional therapies such as transarterial chemoembolization (TACE) and transarterial radioembolization (TARE) are central to disease management. This abstract provides a comparative overview of patient selection strategies for TACE and TARE, emphasizing integration of liver function, tumor burden, and performance status to optimize outcomes.
Material and Methods: A literature review was conducted using PubMed to identify studies evaluating patient selection criteria for TACE and TARE. Articles discussing selection frameworks such as the Barcelona Clinic Liver Cancer (BCLC) staging system, Child–Pugh score, Eastern Cooperative Oncology Group (ECOG) status, and radiographic criteria were prioritized. Key trials, including LEGACY, SARAH, DOSISPHERE-01, and TACTICS, were analyzed for patient selection insights.
Results: TACE remains the first-line therapy for intermediate-stage (BCLC B) HCC in patients with preserved liver function (Child–Pugh A/B) and ECOG 0, with studies demonstrating survival benefits and successful downstaging to transplantation criteria. TARE is indicated for unresectable, liver-dominant HCC in patients with Child–Pugh A or early B, ECOG 0–2, and adequate vascular anatomy. Radiation segmentectomy is most effective for early-stage, localized tumors ( < 5 cm), while lobectomy facilitates hypertrophy and tumor control in extensive unilobar disease. Contraindications for both include decompensated cirrhosis (Child–Pugh C), extensive extrahepatic disease, and uncorrectable arteriovenous shunting. Personalized dosimetry for TARE, as demonstrated in DOSISPHERE-01, has improved tumor control and mitigated complications. Across modalities, ECOG performance status remains a critical predictor of tolerance and survival.
Conclusions: Effective patient selection for TACE and TARE requires a multidisciplinary approach incorporating liver function, tumor burden, vascular anatomy, and performance status. TACE is best suited for multinodular disease in transplant-ineligible patients, whereas TARE, especially with personalized dosimetry, offers an alternative for unresectable or anatomically challenging tumors. Optimizing patient selection enhances efficacy, minimizes complications, and supports integration of these modalities into curative or bridging strategies.
Material and Methods: A literature review was conducted using PubMed to identify studies evaluating patient selection criteria for TACE and TARE. Articles discussing selection frameworks such as the Barcelona Clinic Liver Cancer (BCLC) staging system, Child–Pugh score, Eastern Cooperative Oncology Group (ECOG) status, and radiographic criteria were prioritized. Key trials, including LEGACY, SARAH, DOSISPHERE-01, and TACTICS, were analyzed for patient selection insights.
Results: TACE remains the first-line therapy for intermediate-stage (BCLC B) HCC in patients with preserved liver function (Child–Pugh A/B) and ECOG 0, with studies demonstrating survival benefits and successful downstaging to transplantation criteria. TARE is indicated for unresectable, liver-dominant HCC in patients with Child–Pugh A or early B, ECOG 0–2, and adequate vascular anatomy. Radiation segmentectomy is most effective for early-stage, localized tumors ( < 5 cm), while lobectomy facilitates hypertrophy and tumor control in extensive unilobar disease. Contraindications for both include decompensated cirrhosis (Child–Pugh C), extensive extrahepatic disease, and uncorrectable arteriovenous shunting. Personalized dosimetry for TARE, as demonstrated in DOSISPHERE-01, has improved tumor control and mitigated complications. Across modalities, ECOG performance status remains a critical predictor of tolerance and survival.
Conclusions: Effective patient selection for TACE and TARE requires a multidisciplinary approach incorporating liver function, tumor burden, vascular anatomy, and performance status. TACE is best suited for multinodular disease in transplant-ineligible patients, whereas TARE, especially with personalized dosimetry, offers an alternative for unresectable or anatomically challenging tumors. Optimizing patient selection enhances efficacy, minimizes complications, and supports integration of these modalities into curative or bridging strategies.
