Chemoembolizaton/Drug-Eluting Embolics
(24) Refining the Role of TACE in HCC: Patient Populations That May Benefit Beyond BCLC B
Saturday, October 18, 2025
6:00 PM - 7:30 PM East Coast USA Time
Shrina Jasani, BS – Medical Student, The Ohio State University College of Medicine; Israel Ailemen, BS – Medical Student, The Ohio State University College of Medicine; Jad Elharake, MPH – Medical Student, The Ohio State University College of Medicine; Mina Makary, MD – Associate Clinical Professor of Radiology, Department of Radiology, The Ohio State University Medical Center
Purpose: Transarterial chemoembolization (TACE) is the recommended first-line therapy for intermediate-stage hepatocellular carcinoma (HCC) per the Barcelona Clinic Liver Cancer (BCLC) guidelines. However, emerging evidence suggests its utility may extend to carefully selected early- and advanced-stage patients, particularly in combination with systemic agents. This review evaluates recent data supporting expanded indications for TACE and its role beyond traditional BCLC B populations.
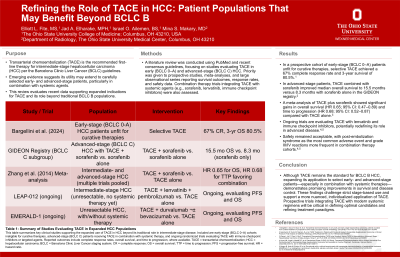
Material and Methods: A literature review was conducted using PubMed and recent consensus guidelines, focusing on studies evaluating TACE in early (BCLC 0–A) and advanced-stage (BCLC C) HCC. Priority was given to prospective studies, meta-analyses, and large observational series reporting survival outcomes, response rates, and safety data. Combination therapy trials integrating TACE with systemic agents (e.g., sorafenib, lenvatinib, immune checkpoint inhibitors) were also assessed.
Results: While primarily recommended for BCLC B disease, TACE has demonstrated meaningful efficacy in other populations. In a prospective cohort of early-stage (BCLC 0–A) patients unfit for curative therapies, selective TACE achieved a 67% complete response rate and 3-year survival of 80.5%. In advanced-stage patients, TACE combined with sorafenib improved median overall survival to 15.5 months versus 8.3 months with sorafenib alone in the GIDEON registrycancers. A meta-analysis of TACE plus sorafenib showed significant gains in overall survival (HR 0.65; 95% CI: 0.47–0.89) and time to progression (HR 0.68; 95% CI: 0.52–0.87) compared with TACE alone. Ongoing trials are evaluating TACE with lenvatinib and immune checkpoint inhibitors, potentially redefining its role in advanced disease. Safety remained acceptable, with post-embolization syndrome as the most common adverse event and grade III/IV reactions more frequent in combination therapy cohorts.
Conclusions: Although TACE remains the standard for BCLC B HCC, expanding its application to select early- and advanced-stage patients—especially in combination with systemic therapies—demonstrates promising improvements in survival and disease control. These findings challenge strict stage-based use and support a more nuanced, individualized application of TACE. Prospective trials integrating TACE with modern systemic regimens will be critical in defining optimal candidates and refining treatment paradigms.
Material and Methods: A literature review was conducted using PubMed and recent consensus guidelines, focusing on studies evaluating TACE in early (BCLC 0–A) and advanced-stage (BCLC C) HCC. Priority was given to prospective studies, meta-analyses, and large observational series reporting survival outcomes, response rates, and safety data. Combination therapy trials integrating TACE with systemic agents (e.g., sorafenib, lenvatinib, immune checkpoint inhibitors) were also assessed.
Results: While primarily recommended for BCLC B disease, TACE has demonstrated meaningful efficacy in other populations. In a prospective cohort of early-stage (BCLC 0–A) patients unfit for curative therapies, selective TACE achieved a 67% complete response rate and 3-year survival of 80.5%. In advanced-stage patients, TACE combined with sorafenib improved median overall survival to 15.5 months versus 8.3 months with sorafenib alone in the GIDEON registrycancers. A meta-analysis of TACE plus sorafenib showed significant gains in overall survival (HR 0.65; 95% CI: 0.47–0.89) and time to progression (HR 0.68; 95% CI: 0.52–0.87) compared with TACE alone. Ongoing trials are evaluating TACE with lenvatinib and immune checkpoint inhibitors, potentially redefining its role in advanced disease. Safety remained acceptable, with post-embolization syndrome as the most common adverse event and grade III/IV reactions more frequent in combination therapy cohorts.
Conclusions: Although TACE remains the standard for BCLC B HCC, expanding its application to select early- and advanced-stage patients—especially in combination with systemic therapies—demonstrates promising improvements in survival and disease control. These findings challenge strict stage-based use and support a more nuanced, individualized application of TACE. Prospective trials integrating TACE with modern systemic regimens will be critical in defining optimal candidates and refining treatment paradigms.
