Ablative Therapy
(33) Synergism of Adoptive Cell Transfer Therapy and Existing Techniques in Interventional Oncology
Saturday, October 18, 2025
6:00 PM - 7:30 PM East Coast USA Time
Fady Bassem Fayek, B.S. – Medical Student, Sidney Kimmel Medical College; Laxman Singanamala, B.S. – Medical Student, Sidney Kimmel Medical College; Mina Makary, M.D. – Physician, Division of Vascular and Interventional Radiology, Department of Radiology, The Ohio State University Wexner Medical Center
Purpose: Adoptive Cell Transfer (ACT) Therapy, such as CAR-T cell therapy, has emerged as a powerful tool in treating solid and liquid tumors. The purpose of this abstract is to provide background on applications of interventional oncology (IO) in overcoming limitations and enhancing the efficacy of ACT therapy.
Material and Methods: A keyword search was conducted to identify full-text, peer-reviewed journal articles on the concurrent use of IO and ACT therapies. This yielded a 2021 review conducted by Kimura and colleagues describing the current state of IO in precision immunotherapy. Specific examples of emerging techniques were then identified, including a 2024 study by Pan et al. which showed augmentation of ACT therapy using Th9 cells in mouse Non-Small Cell Lung Cancer. An additional study was identified from Ito and colleagues in 2019 which demonstrated that concomitant thermal ablation enhanced the efficacy of adoptive T cell therapy in the treatment of injected colon adenocarcinoma or melanoma in mice.
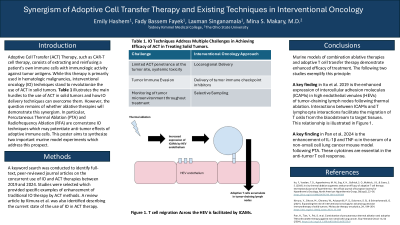
Results: Intravenous delivery of adoptive cells is limited by the extent to which cells can reach the target site and infiltrate the tumor. Furthermore, systemic delivery of adoptive cells can lead to toxicity. Local delivery of adoptive cells by IO can overcome these pitfalls. In addition, IO plays a role in optimizing the tumor microenvironment for ACT. In murine models, percutaneous thermal ablation (PTA) and radiofrequency ablation (RFA) have been shown to increase the release of cytokines due to tumor cell death. These cytokines strengthen the anti-tumor immune responses and help localize CD8+ T-cells to the tumor location. As such, there are speculated roles for intratumoral cytokine delivery to increase adopted T-cell activation without the need for systemic cytokine delivery. Similarly, Phase I clinical trials have shown that immune checkpoint inhibitors potentiate CAR-T cell therapy, with intratumoral delivery of these inhibitors posing a major advantage. Finally, irreversible electroporation performed by IO has been shown to reverse immune checkpoint inhibition, demonstrating yet another synergism of IO and ACT.
Conclusions: Interventional oncology has enormous potential in establishing immune-adjuvant therapies involving ACTs. Human studies are required to validate the efficacy and practicality of approaches used in murine models. Combining tumor ablative and local-delivery ACT therapies are a likely next step in advancing the role of interventional oncology in targeted cancer immunotherapy.
Material and Methods: A keyword search was conducted to identify full-text, peer-reviewed journal articles on the concurrent use of IO and ACT therapies. This yielded a 2021 review conducted by Kimura and colleagues describing the current state of IO in precision immunotherapy. Specific examples of emerging techniques were then identified, including a 2024 study by Pan et al. which showed augmentation of ACT therapy using Th9 cells in mouse Non-Small Cell Lung Cancer. An additional study was identified from Ito and colleagues in 2019 which demonstrated that concomitant thermal ablation enhanced the efficacy of adoptive T cell therapy in the treatment of injected colon adenocarcinoma or melanoma in mice.
Results: Intravenous delivery of adoptive cells is limited by the extent to which cells can reach the target site and infiltrate the tumor. Furthermore, systemic delivery of adoptive cells can lead to toxicity. Local delivery of adoptive cells by IO can overcome these pitfalls. In addition, IO plays a role in optimizing the tumor microenvironment for ACT. In murine models, percutaneous thermal ablation (PTA) and radiofrequency ablation (RFA) have been shown to increase the release of cytokines due to tumor cell death. These cytokines strengthen the anti-tumor immune responses and help localize CD8+ T-cells to the tumor location. As such, there are speculated roles for intratumoral cytokine delivery to increase adopted T-cell activation without the need for systemic cytokine delivery. Similarly, Phase I clinical trials have shown that immune checkpoint inhibitors potentiate CAR-T cell therapy, with intratumoral delivery of these inhibitors posing a major advantage. Finally, irreversible electroporation performed by IO has been shown to reverse immune checkpoint inhibition, demonstrating yet another synergism of IO and ACT.
Conclusions: Interventional oncology has enormous potential in establishing immune-adjuvant therapies involving ACTs. Human studies are required to validate the efficacy and practicality of approaches used in murine models. Combining tumor ablative and local-delivery ACT therapies are a likely next step in advancing the role of interventional oncology in targeted cancer immunotherapy.
