Periportal Nerve Block Enabling Moderate Sedation During Microwave Ablation of Hepatocellular Carcinoma
(26) Periportal Nerve Block Enabling Moderate Sedation During Microwave Ablation ofHepatocellular Carcinoma
Saturday, October 18, 2025
6:00 PM - 7:30 PM East Coast USA Time
Vedant Garg, BS- University of Florida College of Medicine, Gainesville, FL; Grid A Adler, MD- Department of Radiology, University of Florida Health Jacksonville, Jacksonville, FL; Renato Abu Hana, MD- Department of Radiology, University of Florida Health Jacksonville, Jacksonville, FL
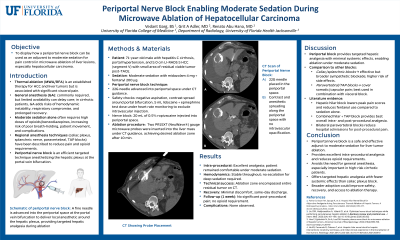
Purpose: Patients with hepatocellular carcinoma (HCC) frequently have advanced cirrhosis and portal hypertension, making them poor candidates for general anesthesia during liver-directed therapies. Ablation procedures are often associated with significant pain, which typically necessitates deep sedation or anesthesia. This report describes the use of a periportal nerve block to enable safe and effective moderate sedation during microwave ablation of HCC.
Material and Methods: A 71-year-old male with hepatitis C–related cirrhosis and a 5.0-cm LI-RADS 5 HCC in hepatic segment V was referred for local therapy after being deemed ineligible for resection or transplantation. To avoid general anesthesia, a periportal nerve block was performed under combined CT and ultrasound guidance. A 22G Pajunk needle was advanced into the porta hepatis, aspiration confirmed no vascular entry, and a small test injection of contrast verified appropriate positioning. Incremental doses of lidocaine with epinephrine and ropivacaine were administered, followed by hydrodissection with D5W to optimize safety and block coverage.
Results: Following the block, two microwave probes were placed under image guidance, achieving an ablation zone of approximately 5.0 × 4.6 cm. Moderate sedation (midazolam 4 mg, fentanyl 200 mcg) was sufficient to complete the procedure without escalation to general anesthesia. The patient remained hemodynamically stable, reported excellent analgesia intra-procedurally, and had minimal discomfort during recovery. No immediate complications were observed, and the patient was discharged the same day.
Conclusions: This case highlights the feasibility of periportal nerve block as an adjunct to enable moderate sedation for ablation of HCC in patients with cirrhosis. By reducing reliance on general anesthesia, this approach may improve procedural safety, shorten recovery, and expand access to ablation in high-risk patients or settings with limited anesthesia resources. Compared with more established techniques such as celiac plexus block, the periportal approach provides targeted hepatic analgesia with minimal systemic effects. Broader adoption and systematic evaluation are warranted to define its role in interventional oncology.
Material and Methods: A 71-year-old male with hepatitis C–related cirrhosis and a 5.0-cm LI-RADS 5 HCC in hepatic segment V was referred for local therapy after being deemed ineligible for resection or transplantation. To avoid general anesthesia, a periportal nerve block was performed under combined CT and ultrasound guidance. A 22G Pajunk needle was advanced into the porta hepatis, aspiration confirmed no vascular entry, and a small test injection of contrast verified appropriate positioning. Incremental doses of lidocaine with epinephrine and ropivacaine were administered, followed by hydrodissection with D5W to optimize safety and block coverage.
Results: Following the block, two microwave probes were placed under image guidance, achieving an ablation zone of approximately 5.0 × 4.6 cm. Moderate sedation (midazolam 4 mg, fentanyl 200 mcg) was sufficient to complete the procedure without escalation to general anesthesia. The patient remained hemodynamically stable, reported excellent analgesia intra-procedurally, and had minimal discomfort during recovery. No immediate complications were observed, and the patient was discharged the same day.
Conclusions: This case highlights the feasibility of periportal nerve block as an adjunct to enable moderate sedation for ablation of HCC in patients with cirrhosis. By reducing reliance on general anesthesia, this approach may improve procedural safety, shorten recovery, and expand access to ablation in high-risk patients or settings with limited anesthesia resources. Compared with more established techniques such as celiac plexus block, the periportal approach provides targeted hepatic analgesia with minimal systemic effects. Broader adoption and systematic evaluation are warranted to define its role in interventional oncology.
