Future Procedures
(80) Thermal Ablation in Papillary Thyroid Carcinoma: Bridging the Gap between Surgery and Active Surveillance
Saturday, October 18, 2025
6:00 PM - 7:30 PM East Coast USA Time
Shrina Jasani, BS – Medical Student, The Ohio State University College of Medicine; Elliott Fite, MS – Medical Student, The Ohio State University College of Medicine; Mina Makary, MD – Associate Clinical Professor of Radiology, Department of Radiology, The Ohio State University Medical Center
Purpose: The standard of care for localized papillary thyroid microcarcinoma (PTMC), defined as tumors ≤1.0 cm or T1aN0M0, is surgery (thyroid lobectomy) or active surveillance (AS) according to most recent guidelines.1 This abstract will explore the use of thermal ablation (TA), primarily radiofrequency ablation (RFA), as an effective treatment option for PTMC.
Material and Methods: A literature review was conducted using PubMed and Embase to identify prospective clinical trials, retrospective and systematic reviews, and meta-analyses evaluating the effectiveness of RFA, microwave ablation (MWA) and laser ablation (LA) compared to surgery and AS for the treatment of PTMC. Outcomes assessed included disease progression rate, volume reduction rate, quality of life (QoL), conversion to surgery, and complication rates.
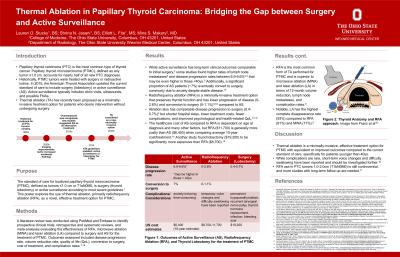
Results: While active surveillance has long-term outcomes comparable to initial surgery, some studies found higher rates of lymph node metastases and disease progression rates between 6.9-9.6% that may be even higher in those < 40yo. Additionally, a significant proportion of patients eventually chose to undergo surgery despite stable disease, likely due to anxiety. Thermal ablation is a minimally-invasive treatment option that preserves thyroid function and has lower progression of disease (0-3.1%) and conversion to surgery (0-1.1%)3,5 compared to AS. Compared to surgery, ablation has equivalent disease progression but shorter hospital stays, lower treatment costs, rates of complications (ex: hypothyroidism), and improved psychological and health-related QoL.5,6,7 RFA is the most common form of TA performed for PTMC and is superior to MWA and LA in terms of 12-month volume reduction, lymph node metastases, and complication rates. Notably, LA has the highest complete disappearance rate (93%) compared to RFA (81%) and MWA (71%).
Conclusions: Thermal ablation is a minimally-invasive, effective treatment option for PTMC with equivalent or improved oncologic outcomes compared to the current standard of care. While complications are rare, short-term voice changes and difficulty swallowing have been reported and should be studied further. RFA use in PTC tumors 1.0-2.0cm (T1bN0M0) is still controversial, and more studies with long-term follow up are needed.
Material and Methods: A literature review was conducted using PubMed and Embase to identify prospective clinical trials, retrospective and systematic reviews, and meta-analyses evaluating the effectiveness of RFA, microwave ablation (MWA) and laser ablation (LA) compared to surgery and AS for the treatment of PTMC. Outcomes assessed included disease progression rate, volume reduction rate, quality of life (QoL), conversion to surgery, and complication rates.
Results: While active surveillance has long-term outcomes comparable to initial surgery, some studies found higher rates of lymph node metastases and disease progression rates between 6.9-9.6% that may be even higher in those < 40yo. Additionally, a significant proportion of patients eventually chose to undergo surgery despite stable disease, likely due to anxiety. Thermal ablation is a minimally-invasive treatment option that preserves thyroid function and has lower progression of disease (0-3.1%) and conversion to surgery (0-1.1%)3,5 compared to AS. Compared to surgery, ablation has equivalent disease progression but shorter hospital stays, lower treatment costs, rates of complications (ex: hypothyroidism), and improved psychological and health-related QoL.5,6,7 RFA is the most common form of TA performed for PTMC and is superior to MWA and LA in terms of 12-month volume reduction, lymph node metastases, and complication rates. Notably, LA has the highest complete disappearance rate (93%) compared to RFA (81%) and MWA (71%).
Conclusions: Thermal ablation is a minimally-invasive, effective treatment option for PTMC with equivalent or improved oncologic outcomes compared to the current standard of care. While complications are rare, short-term voice changes and difficulty swallowing have been reported and should be studied further. RFA use in PTC tumors 1.0-2.0cm (T1bN0M0) is still controversial, and more studies with long-term follow up are needed.
