Future Procedures
(45) Targeting Ovarian Cancer: Advancing Precision Therapy with Porphysome Nanotechnology
Saturday, October 18, 2025
6:00 PM - 7:30 PM East Coast USA Time
Ramanpreet Singh, Fourth-Year Medical Student – Medical Student, College of Medicine, Northeast Ohio Medical University; Mina Makary, MD – Director of Scholarly Activity & Research; Director, IR Clerkship; Leader, IR APP Inpatient Service, Department of Radiology, The Ohio State University Wexner Medical Center
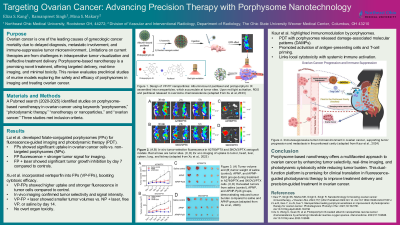
Purpose: Ovarian cancer is one of the leading causes of gynecologic cancer mortality due to delayed diagnosis, metastatic involvement, and immune-suppressive tumor microenvironment. Limitations on current therapies are from challenges in intraoperative tumor visualization and ineffective treatment delivery. Porphysome-based nanotherapy is a promising novel treatment, offering targeted delivery, real-time imaging, and minimal toxicity. This review evaluates preclinical studies of murine models exploring the safety and efficacy of porphysomes in imaging and treating ovarian cancer.
Material and Methods: A Pubmed search (2020-2025) identified studies on porphysome-based nanotherapy in ovarian cancer using keywords “porphysomes,” “photodynamic therapy,” “nanotherapy or nanoparticles,” and “ovarian cancer.” Three studies met inclusion criteria.
Results: Lui et al. developed folate-conjugated porphysomes (FPs) for fluorescence-guided imaging and photodynamic therapy in folate receptor-positive ovarian cancer models. FPs showed significantly greater uptake in the ovarian cancer cells compared to non-targeted porphysomes (NPs). Tumors treated with FPs and laser irradiation showed significantly greater tumor growth inhibition compared to NP and laser and control groups after day 7. Xu et al. expanded by incorporating verteporfin into FPs (VP-FPs), boosting cytotoxic efficacy. In vivo, VP-FPs showed higher uptake and stronger fluorescence in tumor cells compared to the control, confirming higher tumor selectivity and signal intensity. When treated with VP-FP plus laser, tumor volumes were significantly smaller compared to those treated with NP plus laser, free verteporfin, or saline by day 14 (P < 0.01) with no overt toxicity. Kaur et al. highlighted the porphysomes’ potential to modulate the immune system by releasing damage-associated molecular patterns to promote antigen-presenting cells and T-cell priming, bridging between local cytotoxicity and systemic immune activation. This demonstrates its capabilities in imaging and therapy for ovarian cancer.
Conclusions: Porphysome-based nanotherapy offers a multifaceted approach to ovarian cancer by enhancing tumor selectivity, real-time imaging, and photodynamic cytotoxicity while reducing tumor burden. This dual-function platform is promising for clinical translation in fluorescence-guided photodynamic therapy to improve treatment delivery and precision-guided treatment in ovarian cancer.
Material and Methods: A Pubmed search (2020-2025) identified studies on porphysome-based nanotherapy in ovarian cancer using keywords “porphysomes,” “photodynamic therapy,” “nanotherapy or nanoparticles,” and “ovarian cancer.” Three studies met inclusion criteria.
Results: Lui et al. developed folate-conjugated porphysomes (FPs) for fluorescence-guided imaging and photodynamic therapy in folate receptor-positive ovarian cancer models. FPs showed significantly greater uptake in the ovarian cancer cells compared to non-targeted porphysomes (NPs). Tumors treated with FPs and laser irradiation showed significantly greater tumor growth inhibition compared to NP and laser and control groups after day 7. Xu et al. expanded by incorporating verteporfin into FPs (VP-FPs), boosting cytotoxic efficacy. In vivo, VP-FPs showed higher uptake and stronger fluorescence in tumor cells compared to the control, confirming higher tumor selectivity and signal intensity. When treated with VP-FP plus laser, tumor volumes were significantly smaller compared to those treated with NP plus laser, free verteporfin, or saline by day 14 (P < 0.01) with no overt toxicity. Kaur et al. highlighted the porphysomes’ potential to modulate the immune system by releasing damage-associated molecular patterns to promote antigen-presenting cells and T-cell priming, bridging between local cytotoxicity and systemic immune activation. This demonstrates its capabilities in imaging and therapy for ovarian cancer.
Conclusions: Porphysome-based nanotherapy offers a multifaceted approach to ovarian cancer by enhancing tumor selectivity, real-time imaging, and photodynamic cytotoxicity while reducing tumor burden. This dual-function platform is promising for clinical translation in fluorescence-guided photodynamic therapy to improve treatment delivery and precision-guided treatment in ovarian cancer.
