Hepatocellular Carcinoma
(38) Expanding Horizons: Evolving Paradigms in Locoregional Therapy for Recurrent and Residual Hepatocellular Carcinoma
Saturday, October 18, 2025
6:00 PM - 7:30 PM East Coast USA Time
Mina Makary, MD – Division of Interventional Radiology, Department of Radiology, The Ohio State University Wexner Medical Center
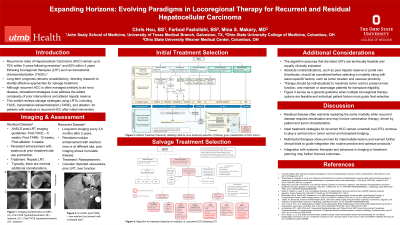
Purpose: Recurrence rates of Hepatocellular Carcinoma (HCC) remain up to 70% within 5 years following resection and 62% within 3 years following locoregional therapies (LRT) such as transarterial chemoembolization (TACE). Thus, long-term prognosis remains unsatisfactory, directing research to identify effective approaches for salvage treatment. Although recurrent HCC is often managed similar to de novo disease, retreatment strategies must address the added complexity of prior interventions and altered hepatic reserve. This exhibit reviews salvage strategies using LRTs including TACE, transarterial radioembolization (TARE), and ablation, for patients with residual or recurrent HCC after initial intervention.
Material and Methods: This exhibit is based on a targeted review of published studies, clinical trials, and institutional protocols, focusing on LRT in the setting of residual or recurrent disease. Key themes and decision points, including imaging assessment, ECOG status, liver function, vascular access, and tumor biology, were consolidated into an algorithmic framework that reflects current evidence and clinical rationale.
Results: This exhibit will outline the BCLC staging and other scoring systems that serve to stratify patients for treatment. Imaging findings suggestive of viable residual or recurrent intrahepatic tumors will be reviewed. Treatment selection, including repeat vs. alternative LRT modalities, will be discussed in the context of tumor burden, hepatic reserve, contraindications, and transplant eligibility. Additional consideration will be given to complex or borderline cases suggesting a need for combination strategies or multimodal therapy.
Conclusions: Locoregional therapies remain critical in the management of residual and recurrent HCC, offering a viable path for intrahepatic tumor control even after treatment failure. Residual viability following initial LRT often warrants repeat treatments with the same modalities. In contrast, recurrent disease may require reassessment, potentially involving a shift in treatment approach or combination therapies. Tailoring LRT strategies with combination or repeat therapies based on imaging, liver function, tumor biology, and prior interventions is essential to optimizing outcomes and extending candidacy for curative options such as transplantation.
Material and Methods: This exhibit is based on a targeted review of published studies, clinical trials, and institutional protocols, focusing on LRT in the setting of residual or recurrent disease. Key themes and decision points, including imaging assessment, ECOG status, liver function, vascular access, and tumor biology, were consolidated into an algorithmic framework that reflects current evidence and clinical rationale.
Results: This exhibit will outline the BCLC staging and other scoring systems that serve to stratify patients for treatment. Imaging findings suggestive of viable residual or recurrent intrahepatic tumors will be reviewed. Treatment selection, including repeat vs. alternative LRT modalities, will be discussed in the context of tumor burden, hepatic reserve, contraindications, and transplant eligibility. Additional consideration will be given to complex or borderline cases suggesting a need for combination strategies or multimodal therapy.
Conclusions: Locoregional therapies remain critical in the management of residual and recurrent HCC, offering a viable path for intrahepatic tumor control even after treatment failure. Residual viability following initial LRT often warrants repeat treatments with the same modalities. In contrast, recurrent disease may require reassessment, potentially involving a shift in treatment approach or combination therapies. Tailoring LRT strategies with combination or repeat therapies based on imaging, liver function, tumor biology, and prior interventions is essential to optimizing outcomes and extending candidacy for curative options such as transplantation.
