Renal Cell Carcinoma
(35) Revolutionizing Renal Tumor Ablation: CEUS-MRI Fusion for Sub-Centimeter Precision
Saturday, October 18, 2025
6:00 PM - 7:30 PM East Coast USA Time
Bo DeVries, B.S. – Medical Student, The University of Toledo College of Medicine; Mustaqueem Pallumeera, B.S. – Medical Student, The Ohio State University College of Medicine; Mina Makary, M.D. – Associate Clinical Professor of Radiology, Department of Radiology, The Ohio State University College of Medicine
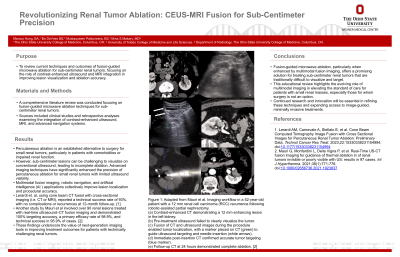
Purpose: To review current techniques and outcomes of fusion-guided microwave ablation for sub-centimeter renal tumors, focusing on the role of contrast-enhanced ultrasound (CEUS) and MRI integration in improving lesion visualization and ablation accuracy.
Material and Methods: A comprehensive literature review was conducted focusing on fusion-guided microwave ablation techniques for sub-centimeter renal tumors. Sources included clinical studies and retrospective analyses examining the integration of contrast-enhanced ultrasound, MRI, and advanced navigation systems.
Results: Percutaneous ablation is an established alternative to surgery for small renal tumors, particularly in patients with comorbidities or impaired renal function. However, sub-centimeter lesions can be challenging to visualize on conventional ultrasound, leading to incomplete ablation. Advanced imaging techniques have significantly enhanced the precision of percutaneous ablation for small renal tumors with limited ultrasound visibility. Multimodal fusion imaging, robotic navigation, and artificial intelligence (AI) applications collectively improve lesion localization and procedural accuracy. One study using cone beam CT fused with cross-sectional imaging (i.e. CT or MRI) reported a technical success rate of 93%, with no complications or recurrences at 12-month follow-up. Another analysis of over 90 renal lesions treated with real-time CEUS–CT fusion imaging demonstrated 100% targeting accuracy, a primary efficacy rate of 98.9%, and technical success in 95.9% of cases. These findings underscore the value of next-generation imaging tools in improving treatment outcomes for patients with technically challenging renal tumors.
Conclusions: Fusion-guided microwave ablation—particularly when enhanced by multimodal fusion imaging—offers a promising solution for treating sub-centimeter renal tumors that are traditionally difficult to visualize and target. This educational review highlights the evolving role of multimodal imaging in elevating the standard of care for patients with small renal masses, especially those for whom surgery is not an option. Continued research and innovation will be essential in refining these techniques and expanding access to image-guided, minimally invasive treatments.
Material and Methods: A comprehensive literature review was conducted focusing on fusion-guided microwave ablation techniques for sub-centimeter renal tumors. Sources included clinical studies and retrospective analyses examining the integration of contrast-enhanced ultrasound, MRI, and advanced navigation systems.
Results: Percutaneous ablation is an established alternative to surgery for small renal tumors, particularly in patients with comorbidities or impaired renal function. However, sub-centimeter lesions can be challenging to visualize on conventional ultrasound, leading to incomplete ablation. Advanced imaging techniques have significantly enhanced the precision of percutaneous ablation for small renal tumors with limited ultrasound visibility. Multimodal fusion imaging, robotic navigation, and artificial intelligence (AI) applications collectively improve lesion localization and procedural accuracy. One study using cone beam CT fused with cross-sectional imaging (i.e. CT or MRI) reported a technical success rate of 93%, with no complications or recurrences at 12-month follow-up. Another analysis of over 90 renal lesions treated with real-time CEUS–CT fusion imaging demonstrated 100% targeting accuracy, a primary efficacy rate of 98.9%, and technical success in 95.9% of cases. These findings underscore the value of next-generation imaging tools in improving treatment outcomes for patients with technically challenging renal tumors.
Conclusions: Fusion-guided microwave ablation—particularly when enhanced by multimodal fusion imaging—offers a promising solution for treating sub-centimeter renal tumors that are traditionally difficult to visualize and target. This educational review highlights the evolving role of multimodal imaging in elevating the standard of care for patients with small renal masses, especially those for whom surgery is not an option. Continued research and innovation will be essential in refining these techniques and expanding access to image-guided, minimally invasive treatments.
