Hepatocellular Carcinoma
(29) Avascular Transformation of Hepatocellular Carcinoma with Systemic Immunotherapy
Saturday, October 18, 2025
6:00 PM - 7:30 PM East Coast USA Time
Ali Yalcintepe, MD – Resident, Radiology, Detroit Medical Center; Alexander Eskandarian, B.S. – Medical Student, Wayne State University School of Medicine; Karan Singh, MD – Interventional Radiology Section Chief, Interventional Radiology, John D. Dingell VAMC; Jeffrey Critchfield, MD – Principal Investigator/Faculty, Interventional Radiology/Radiology, Karmanos Cancer Institute
Purpose: The combination of local embolization and immunotherapy for hepatocellular carcinoma (HCC) is an expanding field. While atezolizumab and bevacizumab therapy is considered the gold standard for immunotherapy, the STRIDE regimen, a dual immunotherapy therapy consisting of a priming dose of tremelimumab (anti-CTLA-4) with monthly durvalumab (anti-PD-L1), has grown in use. We present a unique case of a patient who was unintentionally initiated on STRIDE regimen between mapping angiography and embolization, which seemingly led to rapid avascular tumor transformation.
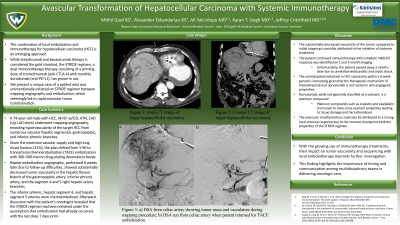
Material and Methods: A 74-year-old male with HCC, HFrEF w/ICD, HTN, CAD (s/p LAD stent) underwent mapping angiography, revealing hypervascularity of the large target HCC from numerous vascular hepatic segmental, gastroepiploic, and inferior phrenic branches. Given the extensive vascular supply and high lung shunt fraction (12%), the plan shifted from Y-90 to transarterial chemoembolization (TACE) embolization with 300–500-micron drug-eluting doxorubicin beads.
Repeat embolization angiography, performed 6 weeks later due to follow-up difficulties, showed substantially decreased tumor vascularity in the hepatic flexure branch of the gastroepiploic artery, inferior phrenic artery, and the segment 4 and 5 right hepatic artery branches. The inferior phrenic, hepatic segment 4, and hepatic segment 5 arteries were chemoembolized. Afterward, discussion with the patient’s oncologist revealed that the STRIDE regimen had been initiated under the assumption that embolization had already occurred, with the last dose 7 days prior.
Results: The substantially decreased vascularity of the tumor compared to initial mapping is possibly attributed to the initiation of systemic treatment. The patient continued immunotherapy with complete mRECIST response was identified on 1 and 3 month imaging. Unfortunately, the patient passed away 3 months later due to unrelated endocarditis and septic shock.
Conclusions: The unanticipated reduction in HCC vascularity within a 6-week period is interesting given that the therapeutic mechanism of tremelimumab and durvalumab is not rooted in anti-angiogenic properties. This finding highlights the importance of timing and communication among multidisciplinary teams in delivering oncologic care. With the growing use of immunotherapy treatments, their impact on tumor vascularity and sequencing with local embolotherapy warrants further investigation.
Material and Methods: A 74-year-old male with HCC, HFrEF w/ICD, HTN, CAD (s/p LAD stent) underwent mapping angiography, revealing hypervascularity of the large target HCC from numerous vascular hepatic segmental, gastroepiploic, and inferior phrenic branches. Given the extensive vascular supply and high lung shunt fraction (12%), the plan shifted from Y-90 to transarterial chemoembolization (TACE) embolization with 300–500-micron drug-eluting doxorubicin beads.
Repeat embolization angiography, performed 6 weeks later due to follow-up difficulties, showed substantially decreased tumor vascularity in the hepatic flexure branch of the gastroepiploic artery, inferior phrenic artery, and the segment 4 and 5 right hepatic artery branches. The inferior phrenic, hepatic segment 4, and hepatic segment 5 arteries were chemoembolized. Afterward, discussion with the patient’s oncologist revealed that the STRIDE regimen had been initiated under the assumption that embolization had already occurred, with the last dose 7 days prior.
Results: The substantially decreased vascularity of the tumor compared to initial mapping is possibly attributed to the initiation of systemic treatment. The patient continued immunotherapy with complete mRECIST response was identified on 1 and 3 month imaging. Unfortunately, the patient passed away 3 months later due to unrelated endocarditis and septic shock.
Conclusions: The unanticipated reduction in HCC vascularity within a 6-week period is interesting given that the therapeutic mechanism of tremelimumab and durvalumab is not rooted in anti-angiogenic properties. This finding highlights the importance of timing and communication among multidisciplinary teams in delivering oncologic care. With the growing use of immunotherapy treatments, their impact on tumor vascularity and sequencing with local embolotherapy warrants further investigation.
