Ablative Therapy
(30) Protecting Adjacent Structures in RCC Ablation: A Case of Combined Pneumodissection and Hydrodissection
Saturday, October 18, 2025
6:00 PM - 7:30 PM East Coast USA Time
Ali Yalcintepe, MD – Resident, Radiology, Detroit Medical Center; Ariana Cho, B.S. – Medical Student, Wayne State University School of Medicine; Hussein Chahrour, MD – Resident, Radiology, Detroit Medical Center; Foaz Kayali, MD – Principal Investigator/Faculty, Radiology, Detroit Medical Center
Purpose: Microwave ablation is a minimally invasive, locoregional therapy that utilizes thermal energy to destroy tumors. Its use for Renal Cell Carcinoma (RCC) is well-studied and it offers shorter hospital stays, faster treatment times, and real-time ultrasound guidance compared to other ablative therapies. Strategies to avoid non-target ablation of close structures such as the bowel, inferior vena cava, collecting system, and body wall include pneumodissection and hydrodissection. In this case, we highlight an Interventional Radiology (IR) treatment approach that leverages pneumodissection and hydrodissection to provide a safe microwave ablation therapy for a RCC tumor.
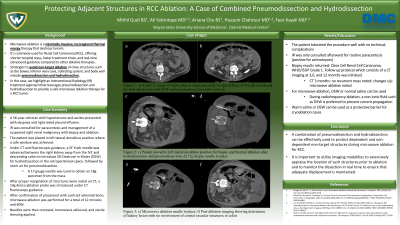
Material and Methods: A 56-year-old man with hypertension and ascites presented with dyspnea and right-sided pleural effusion. IR was consulted for paracentesis and management of a suspected right renal malignancy with biopsy and ablation. The patient was placed in left lateral decubitus position where a safe window was achieved. Under CT and fluoroscopic guidance, a 5F Yueh needle was advanced between the right kidney away from the IVC and descending colon to introduce D5W for hydrodissection in the retroperitoneal space, followed by room air for pneumodissection. A 17 gauge needle was used to obtain an 18g specimen from the mass. After proper margination of structures were noted on CT, a 14g Amica ablation probe was introduced under CT fluoroscopy guidance. After confirmation with contrast administration, microwave ablation was performed for a total of 12 minutes and 40W. Needles were then removed, hemostasis achieved, and sterile dressing applied.
Results: The patient tolerated the procedure well with no complications. IR was only consulted afterwards for a routine diagnostic paracentesis. Biopsy results returned: Clear Cell Renal Cell Carcinoma, WHO/ISUP Grade 1. Follow up protocol which consists of a CT imaging at 3,6, and 12 months was initiated.
Conclusions: A combination of pneumodissection and hydrodissection can be effectively used to protect dependent and non-dependent non-target structures during microwave ablation for RCC. It is important to utilize imaging modalities to extensively appraise the location of such structures prior to ablation and to monitor the dissection in real time to ensure that adequate displacement is maintained.
Material and Methods: A 56-year-old man with hypertension and ascites presented with dyspnea and right-sided pleural effusion. IR was consulted for paracentesis and management of a suspected right renal malignancy with biopsy and ablation. The patient was placed in left lateral decubitus position where a safe window was achieved. Under CT and fluoroscopic guidance, a 5F Yueh needle was advanced between the right kidney away from the IVC and descending colon to introduce D5W for hydrodissection in the retroperitoneal space, followed by room air for pneumodissection. A 17 gauge needle was used to obtain an 18g specimen from the mass. After proper margination of structures were noted on CT, a 14g Amica ablation probe was introduced under CT fluoroscopy guidance. After confirmation with contrast administration, microwave ablation was performed for a total of 12 minutes and 40W. Needles were then removed, hemostasis achieved, and sterile dressing applied.
Results: The patient tolerated the procedure well with no complications. IR was only consulted afterwards for a routine diagnostic paracentesis. Biopsy results returned: Clear Cell Renal Cell Carcinoma, WHO/ISUP Grade 1. Follow up protocol which consists of a CT imaging at 3,6, and 12 months was initiated.
Conclusions: A combination of pneumodissection and hydrodissection can be effectively used to protect dependent and non-dependent non-target structures during microwave ablation for RCC. It is important to utilize imaging modalities to extensively appraise the location of such structures prior to ablation and to monitor the dissection in real time to ensure that adequate displacement is maintained.
