Chemoembolizaton/Drug-Eluting Embolics
(75) Locoregional and Immunotherapy Integration for Hepatocellular Carcinoma: Mechanistic Rationale and Trial Landscape
Saturday, October 18, 2025
6:00 PM - 7:30 PM East Coast USA Time
Jenish Venancius, MPH – Medical Student, The Ohio State University College of Medicine; Alex Rudich, BS – Medical Student, The Ohio State University College of Medicine; Elliott Fite, MS – Medical Student, The Ohio State University College of Medicine; Mina Makary, MD – Associate Clinical Professor of Radiology, Department of Radiology, The Ohio State University Medical Center
Purpose: Immunotherapy and transarterial embolization have synergistic effects in the treatment of hepatocellular carcinoma (HCC) by upregulating tumor antigens and inflammation, therefore increasing susceptibility to immune checkpoint inhibitors such as PD-L inhibitors. This educational review analyzed the rationale and current trial landscape of combined treatment approaches with either transarterial chemoembolization (TACE) or transarterial radioembolization (TARE) and Immunotherapy.
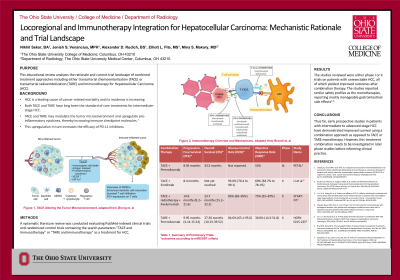
Material and Methods: A systematic literature review was conducted evaluating PubMed-indexed clinical trials and randomized control trials containing the search parameters “TACE and immunotherapy” or “TARE and immunotherapy” as a treatment for HCC. Systematic reviews and meta-analyses were excluded from the search criteria. This yielded a total of 6 studies between 2015-2025.
Results: The studies reviewed were either phase I or II trials on patients with unresectable HCC, all of which yielded improved outcomes after combination therapy. When TACE was combined with pembrolizumab, the objective response rate (ORR) at 12 weeks was 53%, median progression-free survival (PFS) was 8.95 months, and median overall survival (OS) was 33.5 months. A trial using Sintilimab showed an ORR of 30% using RESIST criteria and 60% using mRESIST criteria. A trial employing Avelumabab, TACE, and total radiotherapy found 55% of patients becoming amenable to curative treatment, with 12% undergoing resection or ablation and 42% achieving radiological complete response. Pembroluzimab combined with TARE resulted in a median PFS of 9.95 months (95% CI, 4.14-15.24) and OS 27.30 months (95% CI, 10.15-39.52), with 15 of the 27 patients enrolled being progression free in 6 months. The studies reported similar safety profiles as the monotherapies, reporting mostly manageable gastrointestinal side effects.
Conclusions: Thus far, early prospective studies in patients with intermediate to advanced-stage HCC have demonstrated improved survival using a combination approach versus TACE or TARE monotherapy. However, the treatment regimen needs to be investigated in later phase studies before informing clinical practice.
Material and Methods: A systematic literature review was conducted evaluating PubMed-indexed clinical trials and randomized control trials containing the search parameters “TACE and immunotherapy” or “TARE and immunotherapy” as a treatment for HCC. Systematic reviews and meta-analyses were excluded from the search criteria. This yielded a total of 6 studies between 2015-2025.
Results: The studies reviewed were either phase I or II trials on patients with unresectable HCC, all of which yielded improved outcomes after combination therapy. When TACE was combined with pembrolizumab, the objective response rate (ORR) at 12 weeks was 53%, median progression-free survival (PFS) was 8.95 months, and median overall survival (OS) was 33.5 months. A trial using Sintilimab showed an ORR of 30% using RESIST criteria and 60% using mRESIST criteria. A trial employing Avelumabab, TACE, and total radiotherapy found 55% of patients becoming amenable to curative treatment, with 12% undergoing resection or ablation and 42% achieving radiological complete response. Pembroluzimab combined with TARE resulted in a median PFS of 9.95 months (95% CI, 4.14-15.24) and OS 27.30 months (95% CI, 10.15-39.52), with 15 of the 27 patients enrolled being progression free in 6 months. The studies reported similar safety profiles as the monotherapies, reporting mostly manageable gastrointestinal side effects.
Conclusions: Thus far, early prospective studies in patients with intermediate to advanced-stage HCC have demonstrated improved survival using a combination approach versus TACE or TARE monotherapy. However, the treatment regimen needs to be investigated in later phase studies before informing clinical practice.
