Hepatocellular Carcinoma
(22) The Convergence of Viral Precision and Locoregional Therapy in HCC
Saturday, October 18, 2025
6:00 PM - 7:30 PM East Coast USA Time
Emily Hashem, BS – Medical Student, Sidney Kimmel Medical College, Thomas Jefferson University,111 S 11th St, Philadelphia, PA 19107, United States.; Laxman Singanamala, BS – Medical Student, Sidney Kimmel Medical College, Thomas Jefferson University,111 S 11th St, Philadelphia, PA 19107, United States.; Mina Makary, MD – Physician, Division of Vascular and Interventional Radiology, Department of Radiology, The Ohio State University Wexner Medical Center, 410 West Tenth Avenue, Columbus, OH 43210, United States
Purpose: Oncolytic Virotherapy is a promising therapy for unresectable hepatocellular carcinoma (HCC). This educational exhibit evaluates the latest advances in virotherapy, highlighting the various delivery modalities and the efficacy of virotherapy in combination with other HCC locoregional techniques.
Material and Methods: A review of the published literature covering the use of oncolytic virotherapy in HCC is conducted to identify the latest advances in treatment. Data is collected from the latest clinical and preclinical trials, meta-analyses, and systematic reviews. Findings are presented in text and figure format, comparing the efficacy of different therapies, limitations, and future directions of the field.
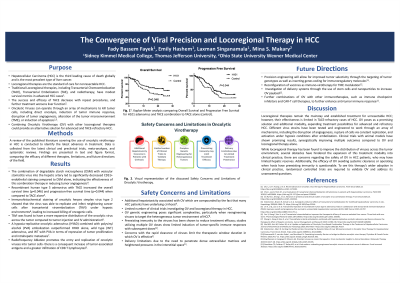
Results: Oncolytic viruses (OV) have demonstrated high accuracy in tumor-targeted cytotoxicity via an array of mechanisms, including direct oncolysis, cell cycle arrest and apoptosis, tumor microenvironment (TME) modulation, and disruption of tumor angiogenesis. Additionally, clinical trials have shown successful synergistic effects of combining Oncolytic Virotherapy with traditional HCC treatment modalities, not only in improving progression-free survival but also improving each other’s therapeutic efficacy; transarterial chemoembolization (TACE) has been found to ameliorate OV therapeutic effects, allowing for enhanced localized delivery of oncolytic viruses and decreasing systemic clearance of the viral load. The horizons of oncolytic virotherapy are promising, with trials investigating precision engineering of OV to tumor genotypes and combination with other immunotherapy regimens. Oncolytic Virotherapy has been halted by challenges pertaining to limited tumor penetration, premature viral elimination, and non-target safety concerns.
Conclusions: Oncolytic virotherapy is a promising constituent in a multimodal therapeutic approach to HCC. Additionally, it is a proponent for a shift towards personalized treatment in interventional oncology. Further research is required to investigate improving treatment efficacy while reducing adverse effects.
Material and Methods: A review of the published literature covering the use of oncolytic virotherapy in HCC is conducted to identify the latest advances in treatment. Data is collected from the latest clinical and preclinical trials, meta-analyses, and systematic reviews. Findings are presented in text and figure format, comparing the efficacy of different therapies, limitations, and future directions of the field.
Results: Oncolytic viruses (OV) have demonstrated high accuracy in tumor-targeted cytotoxicity via an array of mechanisms, including direct oncolysis, cell cycle arrest and apoptosis, tumor microenvironment (TME) modulation, and disruption of tumor angiogenesis. Additionally, clinical trials have shown successful synergistic effects of combining Oncolytic Virotherapy with traditional HCC treatment modalities, not only in improving progression-free survival but also improving each other’s therapeutic efficacy; transarterial chemoembolization (TACE) has been found to ameliorate OV therapeutic effects, allowing for enhanced localized delivery of oncolytic viruses and decreasing systemic clearance of the viral load. The horizons of oncolytic virotherapy are promising, with trials investigating precision engineering of OV to tumor genotypes and combination with other immunotherapy regimens. Oncolytic Virotherapy has been halted by challenges pertaining to limited tumor penetration, premature viral elimination, and non-target safety concerns.
Conclusions: Oncolytic virotherapy is a promising constituent in a multimodal therapeutic approach to HCC. Additionally, it is a proponent for a shift towards personalized treatment in interventional oncology. Further research is required to investigate improving treatment efficacy while reducing adverse effects.
